This is an observational case-control study reported according to STROBE guidelines (see Additional file 1: Checklist S1).
research sample
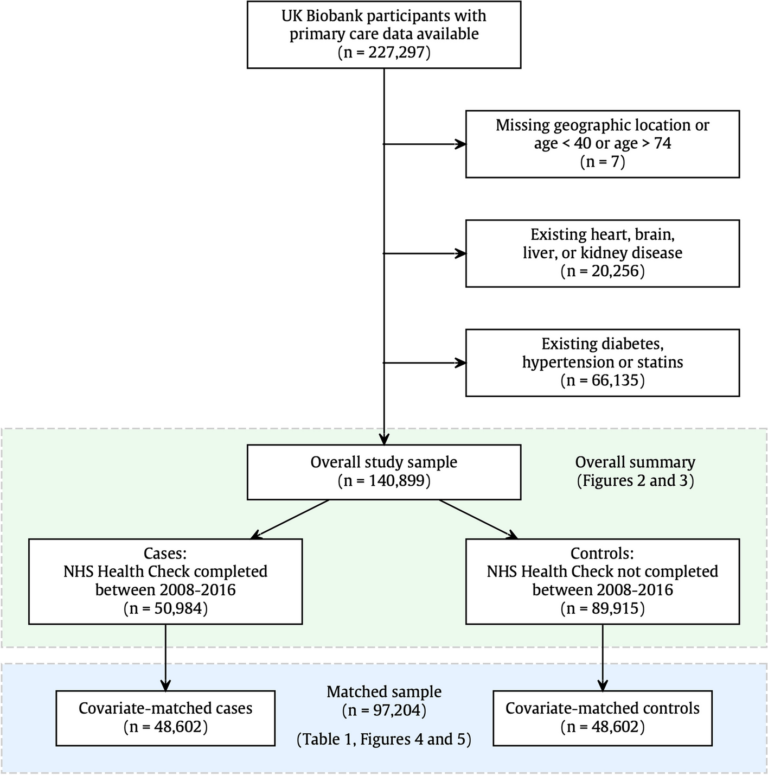
UK Biobank is a UK-wide prospective cohort study with baseline recruitment from March 2006 to October 2010. At the time of this study, 227,297 participants had consented to the release of their primary care records. We reviewed primary care records in the database (Figure 1). Of this participant pool, seven participants either had unknown geographical location or were outside the eligible age range for the NHS health check. A further 20,256 (9%) participants were excluded from the NHS health check due to a pre-existing diagnosis of heart, brain, liver or kidney disease, and 66,135 (31%) were excluded due to a statin prescription or pre-existing diagnosis. Excluded. about diabetes and high blood pressure. NHS health screening standards specifically exclude people with these conditions as they are considered to have already been identified and managed by NHS providers. Therefore, 140,899 participants were used as the study sample.
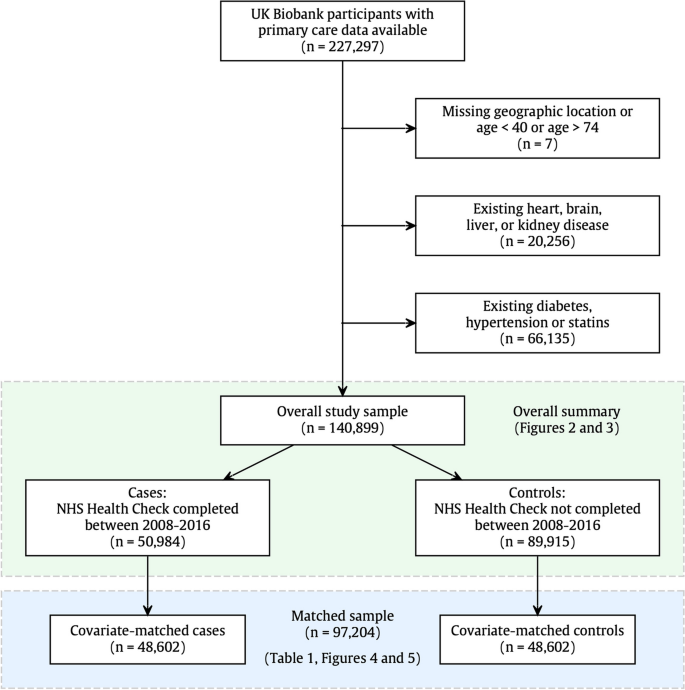
Study sample selection. Participation in this study was dependent on participants having primary care data available and being eligible for an NHS health check. In other words, participants were between 40 and 74 years old and did not have a pre-existing diagnosis that typically requires regular primary care monitoring. Figure 2 shows the overall overview. 2 and 3 relate to the full study sample (n= 140,899), and the outcome modeling is based on the covariate-matched sample (n= 97,204), details are shown in Table 1 and Figure 1. 4 and 5
Case-sensitive matching
To reduce confounding from known sources, we applied an extensive case-control matching algorithm and matched the control group one-to-one with NHS health check recipients using nearest neighbor propensity score matching with a caliper width of 0.2. is created.according to published recommendations [15]. Matching was performed with respect to demographic characteristics (geographic region, age, gender, ethnicity, Townsend Poverty Index, education), family medical history (stroke, heart disease, dementia), and physical measures (BMI, waist-to-hip). It was done. ratio, baseline systolic blood pressure), and health behaviors (smoking, frequency of alcohol intake, physical activity, daily vegetable intake). High-quality matches were obtained in >95% of cases (NHS health check recipients) and unmatched participants were excluded from analysis. When examining excluded participants, we found that although participants tended to be younger, disadvantaged, and obese, the main reason for matching failure was that within the geographic area he needed a one-to-one match. It turns out that there is. In other words, matched controls for London health check recipients must also be from London. From this process, we derived a matched sample of 97,204 participants with 48,602 participants in each exposure group (Figure 1).
Intervention: NHS health check
To identify participants who had undergone an NHS health check (or Scottish equivalent), we performed a text search of primary care clinical records, searching for the following phrases: “Maintaining health, health checkups, testing, healthy start, healthy lifestyle, preventing diabetes, good for men, good for women, good for adults.” This search returned 283,536 records from April 2006 to December 2022. From here, we reviewed the text of the record to exclude other types of health exams (healthy lifestyle, diabetes management, caregiver health exams, and unspecified health exams) and unspecified health exams. Ta. Completion of an NHS health check, for example, invitation (a term that includes invitation, email, letter), neutral descriptors (unsuitable, instructions, status), refusal of a health check (declined, refused, did not attend) ). The remaining codes used to confirm NHS health examinations are provided in Additional file 1: Table S1. The official national rollout took place in April 2009, but up to this date several regions had participated in the pilot program during the year. [16]. Within the UK Biobank his resources, coverage of primary care records was high until mid-2016, but the availability of records declined sharply. Therefore, the exposure period was set between January 1, 2008 and June 30, 2016. The number of recorded health examination exposures by year is shown in Figure 2. For modeling purposes, the exposure date was considered as the first exposure date. I have completed my NHS health check.
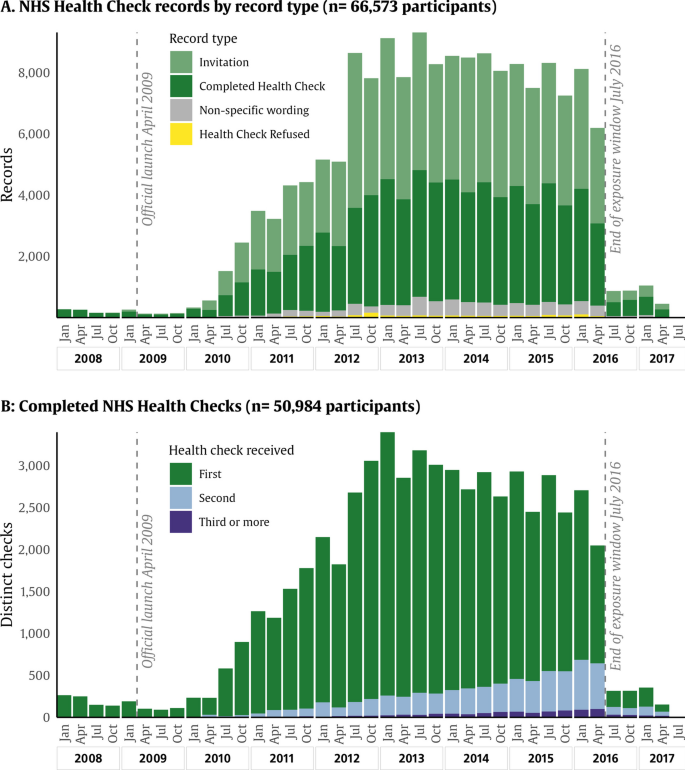
NHS health check records are displayed by year and record type. Distribution describing NHS health check records from UK Biobank. a Distribution of records tagged with NHS Health Exam ID. Color-coded by record type and whether the record describes a completed health exam, an invitation, a decline, or a descriptive tag (which does not necessarily mean completion or decline). B Distribution of completed medical exams. Blue indicates his first NHS medical check recorded, green and yellow indicate follow-up medical checks. Includes participants from January 2008 to July 2016
Confirmation of results
Pre-existing conditions at baseline were assessed both through self-report and linked records (hospital and primary care). Post-baseline onset diseases were identified through records associated with primary care, hospital records, and death registries (Additional file 1: Table S2) using publicly available code lists. Ta. [17,18,19]. We included the following outcomes: hypertension, diabetes, hyperlipidemia, stroke (any type), all-cause dementia, myocardial infarction, atrial fibrillation, heart failure, acute kidney injury, chronic kidney disease (stages 3, 4, or 5), fatty liver disease, alcoholic liver disease, cirrhosis, liver failure, cardiovascular mortality (main cause deaths between ICD I00 and I80), and all-cause mortality. Participants were followed until the end of October 2022. All patient consent procedures were completed by UK Biobank, and details of record linkage at UK Biobank have been previously published. [20].
Definition of covariates
Age, gender, and all other covariates were recorded at baseline. Modeling covariates were selected based on their association with known outcome risk in previous studies. These include age, gender, geographic region, Townsend Poverty Score, ethnicity (white/non-white), post-secondary education (yes/no), body mass index, waist-hip ratio, and current smoking (yes/no). It is included. , systolic blood pressure, Charlson comorbidity index, alcohol frequency, physical activity, and fresh vegetable intake.Charlson comorbidity index was coded from pre-existing conditions at baseline [21]. Physical activity was coded as the sum of metabolic equivalent task minutes per week based on aggregation of the physical activity field according to published guidance. [22]. To divide participants into geographical regions, we identified the coordinates of his six major cities in mainland Britain (London, Bristol, Birmingham, Manchester, Newcastle upon Tyne, and Edinburgh) and based on east and east rounding. We assigned each participant to the nearest city. Northing coordinates are provided at baseline. Some covariates had small amounts of missing values (less than 2%) that were imputed together using multiple imputation with chained equations. [23] (Summary in Additional file 1: Table S3).
statistical analysis
We used graphic illustrations and simple descriptive statistics to outline the characteristics of UK Biobank participants, including primary care data and NHS Health Check utilization. We used two main modeling approaches to assess covariate-adjusted differences in outcomes for health check attendees and non-attendees.
Time-varying Cox regression
We applied Cox survival modeling with interventions (NHS health check dates) coded in a time-varying format, following the method outlined by Therneau et al. [24,25,26]. In this method, follow-up begins at baseline enrollment and all participants begin the follow-up period with intervention-negative status, i.e. without an NHS health check. Then, over time, some participants undergo her NHS health check and receive an intervention positive status on the same day. Survival models were adjusted by the full complement of covariates outlined above recorded at baseline. Although this analysis makes use of the least amount of data and allows time-based differences in exposure effects to be more easily observed, it can still be biased by residual confounding.
Aligned start Cox regression
In this analysis, we adjusted the intervention window between cases and controls in a manner similar to Sebuødegård et al. [27] We then applied proportional hazards regression in the traditional sense. Here, the follow-up period is defined to start from the date of his completed NHS medical examination, and the time of results is also adjusted accordingly. Each control participant (no NHS health check) will be followed up from the corresponding paired intervention date. Complete follow-up periods were compared and there were no significant differences between groups. For alignment start analyses, age was updated to match the intervention date, and remaining covariates were as measured at baseline. This method provides better quality control against known confounds, but comes at the expense of data loss and therefore power loss.
Survival models in both of the above approaches included age, gender, geographic region, Townsend Poverty Score, ethnicity, post-secondary education, BMI, waist-hip ratio, current smoking, systolic blood pressure, Charlson Comorbidity Index, alcohol Adjusted by. Food frequency, physical activity, and fresh vegetable intake. The Aligned-Start model was further adjusted by post-registration period. A multiple testing correction with a 5% false discovery rate was applied to identify significant issues. p-Values across all models.
Further time adjustments
Previous research has found that receipt of an NHS health check is associated with increased detection and diagnosis of prevalent (but unrecognized) diabetes, hypertension, cardiovascular disease and kidney disease. [9]. We therefore performed survival modeling with three exclusion settings: (a) including all outcomes, (b) excluding outcome events in the first 12 months after NHS health check, and (c) excluding NHS NHS Health Check excluding outcome events in the first 24 months after the health check. In epidemiological studies, it is common to exclude events that occur during the first few years of follow-up when studying the relationship between exposure and disease outcome. This incubation period is intended to reduce bias due to reverse causation, which occurs when the main biological processes that produce a disease outcome occur prior to exposure. By excluding events that occur early in follow-up, we hope to observe associations between exposure and disease outcomes that are not due to preexisting conditions that influence exposure status (Rothman et al., p. 218– 219) [28]) and examples [29, 30]. We tested the proportional hazards assumption for the effect of NHS health checks on outcome risk using chi-square tests and graphical representations of Schoenfeld residuals. For sensitivity analyses, we reran the aligned-start Cox model with stratified periods (Therneau and colleagues) [24],section. Four). This approach has the lowest power because each coefficient is calculated using only the results within each time stratum.
unmeasured confounding
lastly, e– The value methodology described by VanderWeele et al. [31] Assess the potential nullifying effects of unobserved confounding variables.I calculated e– We have shown the values and their lower bounds for each significant result and translated these into “age-equivalent years” to help provide an intuitive understanding of relative strength.