This work may not be copied, distributed, displayed, published, reproduced, transmitted, modified, posted, sold, licensed, or used for commercial purposes. By downloading this file, you are agreeing to the publisher’s Terms & Conditions.
ABSTRACT
Objective: To analyze emergency department (ED) mental health presentations over a 7-year period to estimate the timing and magnitude of the seasonal effect across Australia.
Methods: We analyzed data collected by the Australian Institute of Health and Welfare (AIHW) from 2014–2015 to 2020–2021, which included all public hospital ED presentations in Australia that received a mental health diagnosis per the Australian Modification of ICD-10. The data were divided into 4 sequential quarters (Q1 = July–September, Q2 = October–December, Q3 = January–March, Q4 = April–June) and analyzed by sex and age (youth: 18–24 years, adult: 25–64 years, and older adult: > 65 years). Regression analysis was used to assess seasonal variation.
Results: On average, mental health ED presentations were 9% higher in October–December than April–June, which had the lowest rates of mental health ED presentations for males and females. The peak continued into January–March, most prominently for females. Seasonality was evident in the 18–24 and 25–64 age groups. There were increased ED psychiatry presentations in October–December of 14.4% (males) and 9% (females) in the group aged 18–24, as well as increases of 10.3% (males) and 10.1% (females) in those aged 25–64. In January–March, there was an increase in presentations for females of 7% (aged 18–24) and 10.3% (aged 25–64). For adults aged > 65, there were increased presentations in July–September compared to April–June of 4.9% (males) and 3.9% (females).
Conclusions: We found strong, statistically significant peaks in mental health ED presentations in spring and summer. Mental health services need to plan for significantly higher ED mental health demand during these seasons. Further research is required to estimate the size of the mental health seasonal effect in acute hospital settings.
Prim Care Companion CNS Disord 2024;26(1):23m03629
Author affiliations are listed at the end of this article.
“Is the spring coming?” he said. “What is it like?”…
“It is the sun shining on the rain and the rain falling on the sunshine…”
― Frances Hodgson Burnett, The Secret Garden1
Seasonal variation in psychiatric illness has long been of interest. Recent systematic reviews have affirmed the link between the changing seasons and various mental health measures, with spring and summer peaks for suicide rates, hospital admission rates (particularly for bipolar affective disorder–manic phase), and emergency department (ED) self-harm–related presentations.2 These effects have been seen globally across various climates and cultures.2 Spring and summer seasonality of illness in psychiatry contrasts with other medical conditions. For example, there is a winter peak in respiratory virus presentations, as well as heart failure hospital admissions and mortality.3–5 Neurologic conditions such as ischemic stroke, meningitis, and encephalitis also display winter peaks, with varying seasonal peaks for other neurologic conditions.6
Despite identifying the peak season of resource utilization for both mental and physical health conditions, there remains limited research into what effect seasonality might have on ED psychiatric presentations. Rollnik et al7 found seasonal variation over a 2-year study period of ED presentations in California, with peaks in affective, schizophrenia, and adjustment disorders in spring and summer and winter peaks of drug-induced presentations. However, Heboyan et al8 found there was inconclusive evidence for seasonal variation of ED psychiatry presentations over a 3-year study period in Georgia. A limited number of studies found spring and summer peaks of ED presentations of self-harm and suicide attempts.9,10
We aim to address this knowledge gap on seasonality in ED presentations, which has implications for service utilization, resource allocation, service planning, and perhaps community-based preventative approaches. This is particularly pertinent in Anglosphere countries, with current service demand pressures on EDs leading to negative patient outcomes.11 In Australia, mental health–related presentations constituted 3.5% of all ED presentations in 2020–2021, and such presentations have been steadily increasing over the past 15 years.12 Patients presenting for mental health reasons are more likely to have a longer waiting time to initially be seen in EDs and to have a longer ED length of stay compared to all other health presentations, further contributing to hospital access block.12 Similarly, in the United States, there was a 44% increase in ED visits for mental health or substance use disorders between 2006 and 2014.13 Accordingly, analysis of seasonal variation in mental health–related ED presentations is currently needed to inform policy and practice in Australian emergency care.
METHODS
We analyzed the publicly available Australian Institute for Health and Welfare (AIHW) aggregated data relating to ED psychiatry presentations between 2014–2015 and 2020–2021. These data are drawn from the National Non-Admitted Patient Emergency Department Care Database, which maintains data on ED public hospital (not private hospital) presentations across Australia. ED presentations are coded according to the Australian Modification of ICD-10 (ICD-10-AM). For this purpose, mental health is broadly defined to include all presentations with a principal diagnosis within the mental and behavioral disorders chapter of ICD-10-AM (codes F00–F99). The data were delineated by quarter of presentation, with quarter 1 to 4 corresponding to the financial year (ie, Q1 = July–September, Q2 = October–December, Q3 = January–March, Q4 = April–June) as an approximation for the related seasons (winter, spring, summer, autumn). The data were stratified by sex (male and female) and age (18–24, 25–64, ≥ 65). We grouped and organized these data.
Descriptive analysis was followed by regression analysis. On the basis of visual inspection of times series plots, the magnitude of the seasonal fluctuations appeared to be not related to the overall trend level of the series, suggesting that the 2 components were additive (ie, Xt = Trendt + Seasonalt, where Xt is the value of ED presentations at time t). Therefore, to isolate the seasonal effects, a linear regression analysis was performed. Because these were quarterly data, the regression model included a constant term and 3 dummy variables with Q4 ED presentations (April–June) as referent. Also, because interpreting the results as “net of the time trend” is confusing, we performed a regression model where was the sample mean of our time variable. Accordingly, the time variable was centered in the regression model so that estimates of ED presentations for each quarter were interpreted around the midpoint of the series.
Ethics approval was not required or sought as data were publicly available in deidentified aggregate format, approved for release by the Australian federal government through the AIHW.12
RESULTS
There is a consistent trend for increased ED psychiatry presentations in the Australian (southern hemisphere) spring and summer months of October to December and January to March when compared to autumn and winter months of April to June and July to September. Figure 1 shows the seasonal pattern of ED psychiatry presentations throughout the study period, with consistent peaks in spring and summer months and troughs in autumn and winter months.
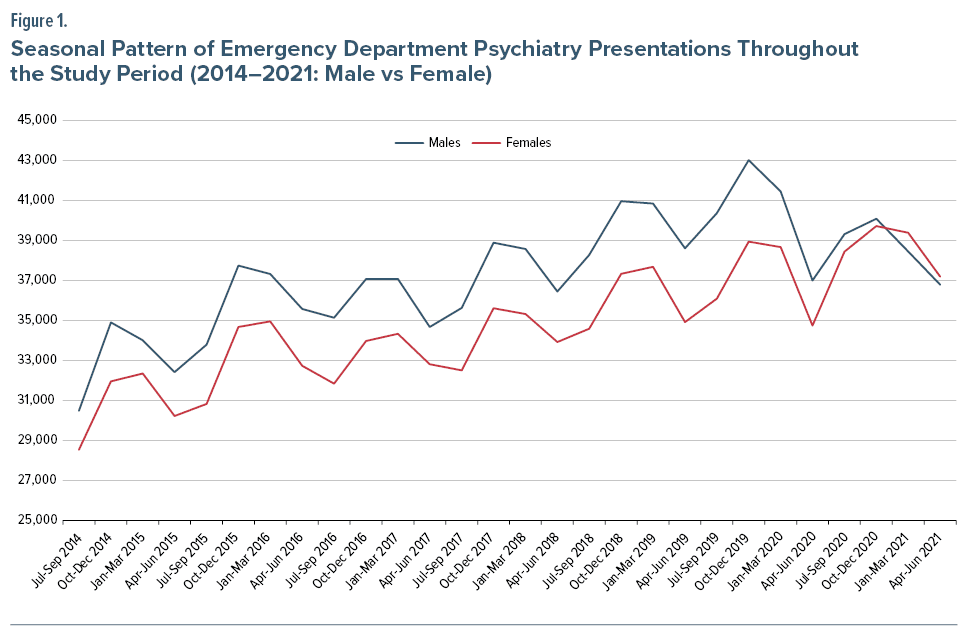
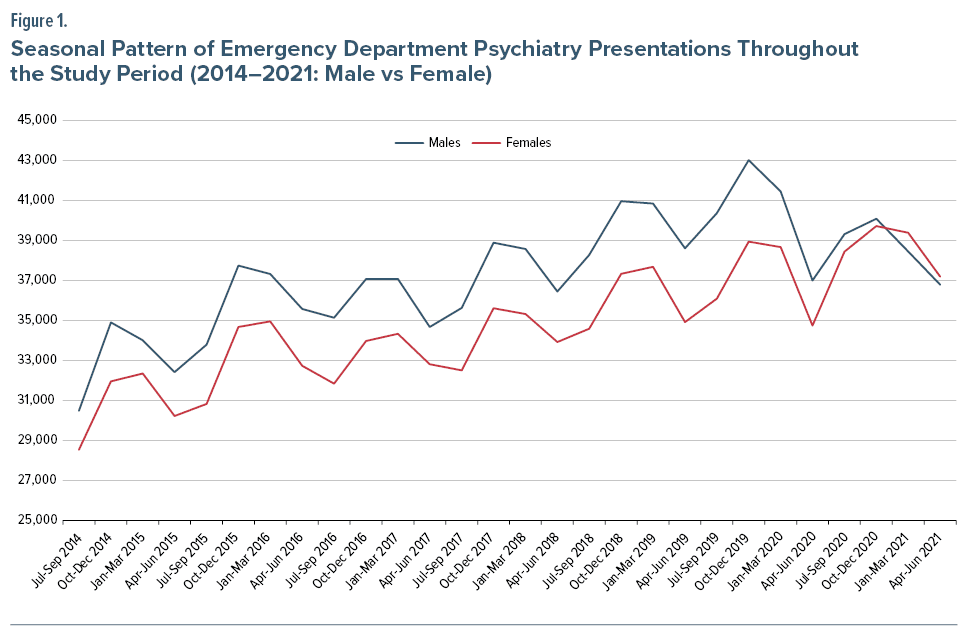
To quantify the seasonal differences, we performed quarterly seasonal calculation of the aggregated difference in numbers of presentations from the autumn quarter baseline, expressed as a percentage, across all 7 years of the study (Table 1). On average, the spring (October–December) quarter psychiatry presentations were 9% to 10% more than the baseline autumn quarter (April–June). This increase continued into the summer (January–March) quarter, with 7.5% more presentations compared to baseline. Seasonal variation amplitude was similar in males and females. Males had a spring presentation peak of 9.98% compared to the autumn baseline, while females showed a summer peak of 7.84%. These findings were consistent for the 18–24 and 25–64 age groups and by sex. Males aged 18–24 years showed a particularly prominent spring peak increase in presentations of 14.38%. Women aged 25–64 years also showed a summer seasonal presentation peak of 10.33%. In contrast, the cohort ≥ 65 years demonstrated winter peaks of 4.92% (males) and 3.85% (females), as well as spring peaks of 4.1% (male) and 6.0% (female). In this age group, there was a smaller amplitude spring seasonal presentation peak and a much smaller summer peak.
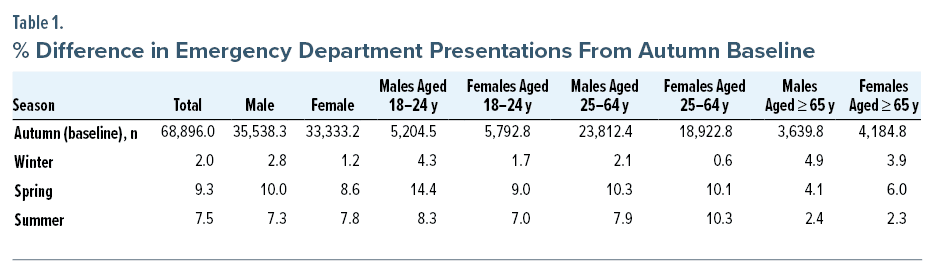
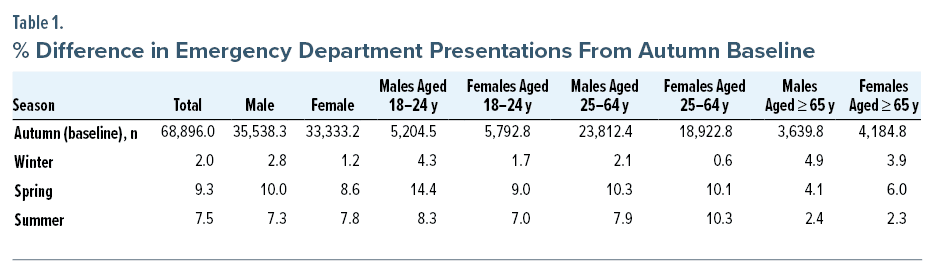
Table 2 shows results of a seasonal linear regression model for ED psychiatry presentations by sex and age group. The time variable is mean-centered; therefore, all estimates are interpreted as around the midpoint of the series for a given quarter. Consistent with the approach to the numerical count data in Table 1, the fourth quarter (corresponding to April–June, ie, autumn) is the referent baseline.
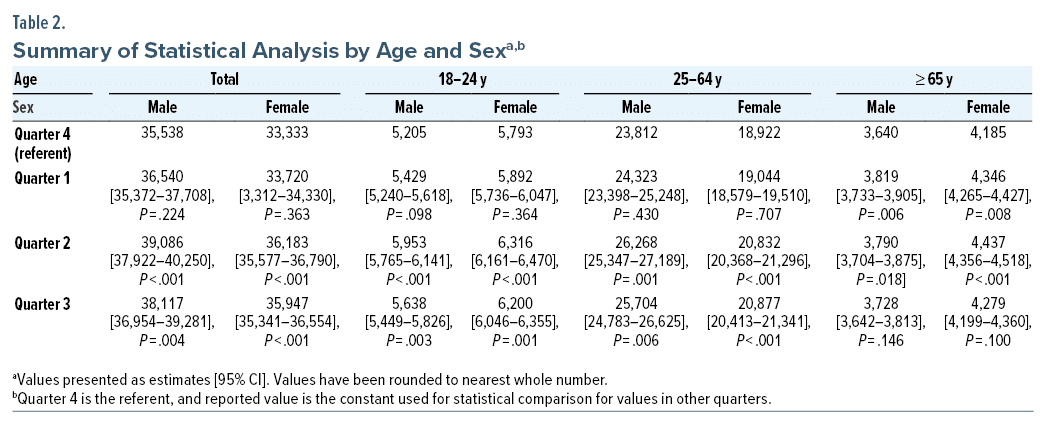
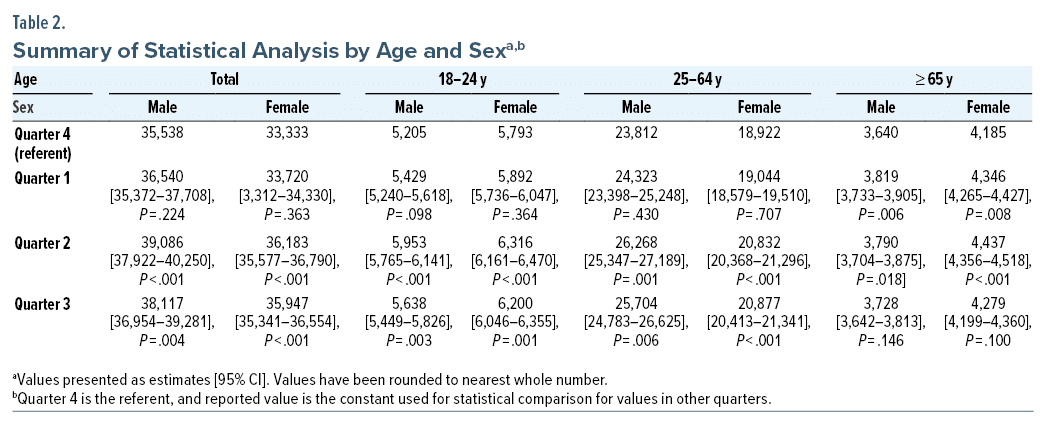
All Age Combined Results by Sex
The estimated means are the average number of ED presentations (see column 2 of Table 2). For males, the average number of ED visits in quarter 4 (referent) is 35,538. The average number of ED visits in quarter 1 is 35,538 + 1,002 = 36,540, and this increase is not statistically significant (P = .224). The average number of ED visits for males in quarter 2 is 39,086 (35,538 + 3,548), and this increase is statistically significant when compared to quarter 4 (P < .001). The average number of ED visits for males in quarter 3 is 38,117 (35,538 + 2,579), which is also a statistically significant increase (P = .004) when compared to quarter 4. Overall, quarter 2 has the largest statistically significant increase in male ED psychiatric presentations followed by quarter 3.
For females of all ages combined, the average number of ED presentations in quarter 4 (referent) is 33,333 (see column 3 of Table 2). The average number of ED visits in quarter 1 is 33,720, and this increase is not statistically significant (P = .363). The average number of ED visits in quarter 2 is 36,183, and this increase is statistically significantly higher than quarter 4 (P < .001). The average number of ED visits in quarter 3 is 35,947 and is also a statistically significant increase in ED visits when compared to quarter 4 (P < .001). Therefore, in females, both quarters 2 and 3 have a statistically significant increase in ED psychiatry presentations.
Age Stratified Results by Sex
For males aged 18–24 years, ED presentations in quarter 1 were not statistically significantly different than in quarter 4 (5,429 vs 5,205, P = .098). There was a statistically significant increase between quarter 2 versus quarter 4 (5,953 vs 5,205, P < .001) and quarter 3 versus quarter 4 (5,638 vs 5,205, P = .003). For females aged 18–24, there was no statistically significant difference in ED presentations in quarter 1 compared to quarter 4 (5,892 vs 5,793, P = .364). There was a statistically significant increase between quarter 2 versus quarter 4 (6,316 vs 5,793, P < .001) and quarter 3 versus quarter 4 (6,200 vs 5,793, P = .001).
For males aged 25–64 years, the average number of ED presentations was not significantly different between quarter 1 versus quarter 4 (24,323 vs 23,812, P = .430). Presentation rates for this cohort in quarter 2 were higher compared to quarter 4 (26,268 vs 23,812, P = .001) and in quarter 3 versus quarter 4 (25,704 vs 23,812, P = .006). A similar pattern of seasonal effects was found for females in this age group (25–64 years) with quarter 4 as referent: a nonsignificant increase in quarter 1 (19,044 vs 18,922, P = .707) and statistically significant increases in quarter 2 (20,832 vs 18,922, P < .001) and quarter 3 (20,877 vs 18,922, P < .001).
For males in the age group ≥ 65 years, there was a statistically significant increase in ED visits in quarter 1 versus quarter 4 (3,819 vs 3,640, P = .006) and quarter 2 versus quarter 4 (3,790 vs 3,640, P = .018). However, there was no statistically significant change in presentations in quarter 3 versus quarter 4 (3,728 vs 3,640, P = .146). A similar trend was also found for females in this age group (≥ 65 years) with quarter 4 as referent: a statistically significant increase in both quarter 1 (4,346 vs 4,185, P = .008) and quarter 2 (4,437 vs 4,185, P < .001). On the other hand, there was no significant change in ED presentation rates for this cohort in quarter 3 (4,279 vs 4,185, P = .100).
DISCUSSION
There was seasonal variation in ED psychiatric presentations consistent with the previous data on seasonal variation of suicide rates, hospital admission rates for mania, and ED presentations for self-harm and suicide attempts. The degree of this seasonal variation is significant in all cohorts < 65 years of age, with a more protracted spring and summer peak for females compared to males (who only demonstrate a statistically significant spring peak).
Factors Affecting Seasonal Variation in ED Psychiatric Presentations
Biological factors. Patterns of seasonal variation in psychiatric presentations may arise for a number of reasons. Various biological factors have been suggested to contribute to seasonality in both suicide and mood variation, with a time-lag effect potentially explaining differing peak seasons.14 Seasonal variation has been reported for multiple neurotransmitter systems, especially seasonal variations in serotonergic and dopaminergic systems, which have biological roles in mood, cognition, and reward signaling.15
Light strongly entrains the human internal clock, leading to modifications in brain function with variation in daylight hours through the year. Therefore, circadian rhythm changes are also likely to mediate seasonal effects. An inability of the circadian rhythm to accommodate to seasonal changes might increase the risk for various mood and behavioral problems.15 This is perhaps best demonstrated through seasonal affective disorder (SAD), wherein a delay in the circadian rhythm might be responsible for the winter depression seen in this condition.16 In turn, this may, through a time-lag effect from winter circadian dysrhythmia, lead to summer presentations to the ED. In Australia, such circadian-related seasonality may be more pronounced in southern states when compared to the tropical northern regions.17
Variation in circadian rhythm is also considered a significant contributor to seasonal variation in ED presentations for people with bipolar affective disorder, who may be affected by light exposure and melatonergic signaling.18 In bipolar affective disorder, there may be a shorter than usual circadian rhythm, both phase-delay and phase-advance in circadian rhythm, and an inherent instability in circadian rhythm that can be prone to desynchronization and disruption.18 This may be linked to melatonergic disruption, with decreased peak melatonin levels in people with bipolar disorder, along with hypersensitive pineal responses to light exposure.18 Chronotropic factors may specifically contribute to the greater seasonal variation we observed in females, who display both greater sensitivity to circadian modulation and seasonal fluctuation in markers of serotonin activity when compared to males.15 Zhang and Volkow15 postulate that the delayed circadian phase in younger adults may drive the more prominent seasonal differences seen in this cohort compared to older adults.
Social factors. Social factors may also contribute to seasonal variation in ED psychiatry presentations. Durkheim first suggested this might contribute to seasonality of suicide rates. He postulated increased interpersonal activity in the clement weather of spring and summer might catalyze interpersonal conflict, which in some individuals may lead to suicidal behavior, situational crises, or exacerbation of underlying psychiatric illnesses or personality vulnerabilities.19 The “broken promises” theory may also contribute to seasonal variation in ED psychiatry presentations. This theory has mainly been suggested to contribute to suicide seasonality, wherein the metaphorical new beginning of spring may fail to live up to an individual’s expectations and lead to suicidal behavior.2 This same mechanism may not only lead to suicidal behavior or ideation, but also contribute to ED presentations through exacerbations of mental illnesses or personality vulnerabilities.
Seasonal variation in employment activity may also contribute to seasonality in ED presentations, particularly in rural areas with large agricultural employment.20,21 This has previously been reflected in studies relating to suicide seasonality, which tends to be most pronounced in agricultural communities, despite increased agricultural activity during spring.21 This seasonality may arise through increased psychological stress in spring due to the importance of the harvest for the overall success of the year, which in turn may be impacted by the climate and various other factors outside of an individual’s control.22
Substance use effects. Seasonal variation in mental health, and in particular ED psychiatric presentations, may arise from seasonal variation in drug and alcohol use. There are summer peaks to alcohol consumption in Australia23 and a prominent summer peak for alcohol-related suicides in coronial data.24 Further data suggest that a spring and summer peak to alcohol use is a worldwide trend, with studies from the Netherlands25 and Norway26 finding spring and summer peaks in alcohol consumption, correlating with sales data showing peaks for alcohol sales in these seasons. The latter of these specifically found that the amplitude of seasonal variation in binge drinking was higher for women than men, which may contribute to the extended summer peak to ED presentations seen in women.26 Summer alcohol consumption peaks have also been found in Switzerland and Canada,27,28 as well as summer peaks for hospital admissions for alcohol-related hepatitis29 in the United States and pancreatitis30 in Wales.
There are scarce seasonal variation data for illicit drug use, although in the United States, Palamar et al31 found that summer is a risk factor for initiation of cannabis, cocaine, LSD, and MDMA, all of which may lead to specific substance-induced ED psychiatric presentations or may be a significant comorbid factor, influencing overall ED psychiatric presentations. Also, wastewater analysis has suggested record high illicit drug consumption is most likely to occur in December in Australia (without specifying any particular drugs),32 while in Canada cannabis and cocaine use both peaked in summer months and codeine was detected at lower levels in late summer.33
Temporal effects. Spring and summer peaks to ED psychiatric presentations may result from time-lagged effects from onset of illness to ED/hospital presentation. Souêtre et al34 suggest that while the lag time for a condition such as mania is quite short (< 1 month), depression may have a lag time of 3–6 months between initial symptom onset and hospital admission. This may account for some of the spring and summer peak to ED psychiatric presentations for depression whose onset may have been in winter,1 but which culminated in ED/hospital presentation a few months later.
Age-related effects. The observed winter and spring peak to ED psychiatric presentations in older adults may arise from different factors compared to those seen in younger people. For example, Australian data suggest that older adults are less likely to engage in high-risk alcohol consumption and to consume illicit drugs than younger adults, while being more likely to be daily drinkers.35 This may contribute to less pronounced seasonal peaks and specifically the lack of summer peaks, given the increased incidence of binge drinking in this season. Older adults are less likely to be engaged in employment than younger people, and they may not experience seasonal employment effects. Finally, there may also be differences in biological factors contributing to ED psychiatry presentations in older adults. Interestingly, Zhang and Volkow15 report that SAD is more prevalent in youth, while the incidence of melancholic depression has also been demonstrated to be similar across various age groups.36,37
Limitations
Our research has some limitations. First, due to the lack of diagnostic categorization in the dataset, it is not possible to determine the diagnoses contributing to the observed seasonal variation.7 Furthermore, while mental health diagnoses included suicidal ideation or self-harm, which may have driven increased seasonal ED presentations, those without an ICD diagnosis were not included. Further studies might encompass all ED presentations for suicidal behavior, given previous studies investigating suicide attempts presenting to the ED.10 Finally, while the country-wide nature of these data represents a strength, it is also a limitation further making etiologic analysis difficult given the wide-ranging climates across different states in Australia. This is particularly the case given the demonstrated higher prevalence of SAD in Tasmania compared to other regions of Australia.17 The majority of the Australian population lives in large cities in coastal temperate zones, so the study results may be most generalizable for those regions on a representativeness basis as the source of the data. Further studies should investigate seasonal variation in each major city of Australia and correlate this with specific climate conditions (eg, rain, sunshine hours, temperature, humidity). This could allow for better understanding of the factors influencing seasonality and assist with implementing more city-specific preventative measures and more targeted service planning.
CONCLUSIONS AND CLINICAL IMPLICATIONS
The findings of this study are relevant in terms of specifically planning for ED psychiatric resourcing and requirements for hospital bed resources. Resources aimed at preventing crises or providing aftercare following ED psychiatric presentations may also benefit from increased resourcing in the spring and summer months. More speculatively, ED presentations may also be minimized through increased primary care resourcing in autumn and winter months, given the potential 3- to 6-month lag between disease onset and ED presentation in some cases. Further research is needed to identify specific etiologic and diagnostic factors contributing to spring and summer seasonality of ED presentation and whether this seasonality is manifest in large Australian cities and, indeed, the rest of the world—particularly in other similar high-income nations.
Article Information
Published Online: February 6, 2024. https://doi.org/10.4088/PCC.23m03629
© 2024 Physicians Postgraduate Press, Inc.
Submitted: August 23, 2023; accepted October 19, 2023.
To Cite: Della DF, Smith D, Looi JCL, et al. Seasonal surge for mental health demand in emergency departments. Prim Care Companion CNS Disord. 2024;26(1):23m03629.
Author Affiliations: College of Medicine and Public Health, Flinders University, Adelaide, South Australia, Australia (Della, Smith, Allison, Bastiampillai); Academic Unit of Psychiatry and Addiction Medicine, The Australian National University School of Medicine and Psychology, Canberra, ACT, Australia (Looi); Consortium of Australian-Academic Psychiatrists for Independent Policy and Research Analysis, Canberra, ACT, Australia (Looi, Allsion, Bastiampillai); Department of Psychiatry, Monash University, Wellington Road, Clayton, VIC, Australia (Bastiampillai).
Corresponding Author: David Della, BParamedicSc, MD, Flinders Medical Centre, Flinders Drive, Bedford Park, SA 5042 (dell0079@flinders.edu.au).
Relevant Financial Relationships: None.
Funding/Support: None.
Clinical Points
- Acute emergency department (ED) psychiatric presentations in Australia show seasonal increases in spring and summer.
- Chronotropic strategies to assist patients in navigating changes in daylength and establishing stable sleep-wake cycles to prevent worsening mental health should be considered.
- There is a potential time-lag effect of worsening psychiatric health in winter months, leading to ED presentations in spring and summer, which may require specific intervention aimed at preventing deterioration to the extent of ED presentation.
- Prevention and treatment of drug and alcohol abuse may also need spring and summer seasonal intervention, if not earlier in winter, as a potential means to reduce related ED psychiatric presentations.


