King County public health officials confirmed Tuesday that the first known outbreak of a certain deadly fungus has struck Washington state.
The fungus, called Candida auris or C. auris, was first discovered in Seattle and the public in July when a Pierce County resident tested positive for the fungus at Kindred Hospital, a long-term acute care hospital in Seattle. According to the Department of Health, this is the first case in the state. King County. No further cases were discovered at that time.
This month, another C. auris infection was confirmed in a patient recently admitted to Kindred, the public health agency said in a blog post. The patient was tested through the state Department of Health's screening program, which promotes early detection of multidrug-resistant bacteria and bacteria that are resistant to treatment, such as C. auris, the post said.
More than a week later, the hospital confirmed three more cases, all of whom had negative fungal tests upon initial admission. That means the state's first confirmed C. auris outbreak started to spread.
Public health officials said they were not yet sure about the initial source of infection, adding: “It may never be identified.” Further information about the patient was not immediately available.
“Public Health continues to work with Kindred to reduce the spread of infection,” the post said. “This includes keeping patients who test positive for C. auris away from other patients to reduce the risk of infection and using specific disinfectant cleaning products that are effective against C. auris. Masu.”
Kindred is in the process of notifying other facilities that previously accepted Kindred patients.
The Centers for Disease Control and Prevention announced last spring that C. auris infections are considered an urgent public health threat and have spread at an “alarming” rate during the coronavirus pandemic. The fungus was first reported in the United States in 2016 and was responsible for a 200% spike in infections from 2019 to 2021, The New York Times reported last year.
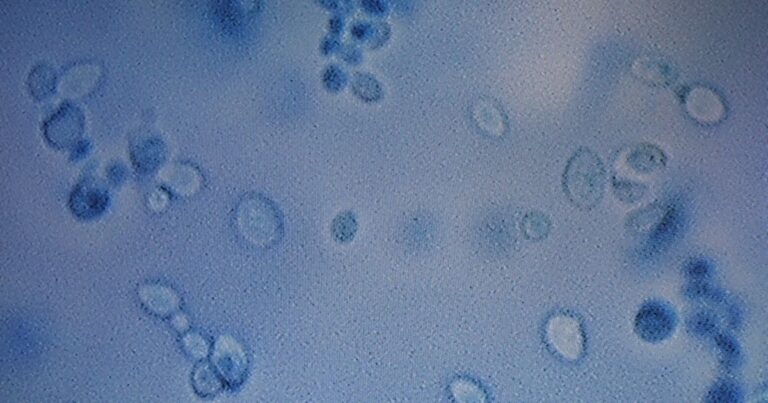
C. auris is of particular concern because it is resistant to common antifungal drugs, Claire Bostrom-Smith, manager of King County's healthcare-associated infectious disease program, said in a blog post. It can also spread throughout the body without the patient showing any symptoms, a process called “colonization,” Bostrom-Smith said.
Bostrom-Smith added that 5% to 10% of patients who become “colonized” with C. auris eventually develop “invasive” infections that can be severe. More than 45% of people who get an invasive infection die within the first 30 days, Bostrom-Smith said.
Bostrom-Smith said people in long-term acute care facilities are generally most at risk, primarily because they are more likely to become critically ill and dependent on equipment such as catheters and breathing tubes. This is because they are doing so.
According to the CDC, C. auris is generally not a threat to healthy people.
Symptoms usually include infection in various parts of the body, including the bloodstream, open wounds, and ears, but it also depends on the location and severity of the infection, according to the CDC. The agency noted that some symptoms may be similar to others caused by the bacteria, adding that “there is no common set of symptoms” specific to C. auris infection.
The fungus can survive for weeks or more on some surfaces, so it can be difficult to remove, even in medical settings, Bostrom-Smith added.
As public health teams have been working with Kindred for months to implement an early testing program, they expected to “eventually find C. auris in Washington,” Tuesday's post said.
According to the Seattle-King County Department of Public Health, “Early detection is the key to controlling the spread of C. auris so prevention strategies can be put in place before it spreads.”