Llovet, J. M. et al. Hepatocellular carcinoma. Nat. Rev. Dis. Primers. 7(1), 6 (2021).
Google Scholar
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Google Scholar
Satriano, L., Lewinska, M., Rodrigues, P. M., Banales, J. M. & Andersen, J. B. Metabolic rearrangements in primary liver cancers: Cause and consequences. Nat. Rev. Gastroenterol. Hepatol. 16(12), 748–766 (2019).
Google Scholar
Wang, C., Cao, Y., Yang, C., Bernards, R. & Qin, W. Exploring liver cancer biology through functional genetic screens. Nat. Rev. Gastroenterol. Hepatol. 18(10), 690–704 (2021).
Google Scholar
Anwanwan, D., Singh, S. K., Singh, S., Saikam, V. & Singh, R. Challenges in liver cancer and possible treatment approaches. Biochim. Biophys. Acta Rev. Cancer. 1873(1), 188314 (2020).
Google Scholar
Calle, E. E., Rodriguez, C., Walker-Thurmond, K. & Thun, M. J. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N. Engl. J. Med. 348(17), 1625–1638 (2003).
Google Scholar
Sohn, W. et al. Obesity and the risk of primary liver cancer: A systematic review and meta-analysis. Clin. Mol. Hepatol. 27(1), 157–174 (2021).
Google Scholar
Larsson, S. C. & Wolk, A. Overweight, obesity and risk of liver cancer: A meta-analysis of cohort studies. Br. J. Cancer. 97(7), 1005–1008 (2007).
Google Scholar
Simon, T. G. et al. Diabetes, metabolic comorbidities, and risk of hepatocellular carcinoma: Results from two prospective cohort studies. Hepatology (Baltimore, Md). 67(5), 1797–1806 (2018).
Google Scholar
Dhar, D., Seki, E. & Karin, M. NCOA5, IL-6, type 2 diabetes, and HCC: The deadly quartet. Cell Metab. 19(1), 6–7 (2014).
Google Scholar
Lee, Y. C. et al. Meta-analysis of epidemiologic studies on cigarette smoking and liver cancer. Int. J. Epidemiol. 38(6), 1497–1511 (2009).
Google Scholar
Bagnardi, V. et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. Br. J. Cancer. 112(3), 580–593 (2015).
Google Scholar
Papadimitriou, N. et al. An umbrella review of the evidence associating diet and cancer risk at 11 anatomical sites. Nat. Commun. 12(1), 4579 (2021).
Google Scholar
Poole, R. et al. Coffee consumption and health: Umbrella review of meta-analyses of multiple health outcomes. BMJ (Clin. Res. Ed). 359, j5024 (2017).
Google Scholar
Ahn, J. et al. Prediagnostic total and high-density lipoprotein cholesterol and risk of cancer. Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol. 18(11), 2814–2821 (2009).
Google Scholar
Wang, Y. et al. Type 2 diabetes and gender differences in liver cancer by considering different confounding factors: A meta-analysis of cohort studies. Ann. Epidemiol. 26(11), 764–772 (2016).
Google Scholar
Davey Smith, G. & Hemani, G. Mendelian randomization: Genetic anchors for causal inference in epidemiological studies. Hum. Mol. Genet. 23(R1), R89-98 (2014).
Google Scholar
Chen, J. et al. The trans-ancestral genomic architecture of glycemic traits. Nat. Genet. 53(6), 840–860 (2021).
Google Scholar
Vujkovic, M. et al. Discovery of 318 new risk loci for type 2 diabetes and related vascular outcomes among 1.4 million participants in a multi-ancestry meta-analysis. Nat. Genet. 52(7), 680–691 (2020).
Google Scholar
Kettunen, J. et al. Genome-wide study for circulating metabolites identifies 62 loci and reveals novel systemic effects of LPA. Nat. Commun. 7, 11122 (2016).
Google Scholar
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51(2), 237–244 (2019).
Google Scholar
Zhong, V. W. et al. A genome-wide association study of bitter and sweet beverage consumption. Hum. Mol. Genet. 28(14), 2449–2457 (2019).
Google Scholar
Sudlow, C. et al. UK biobank: An open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12(3), e1001779 (2015).
Google Scholar
Kurki, M. I., Karjalainen, J., Palta, P., Sipilä, T. P., Kristiansson, K., Donner, K. et al. FinnGen: Unique genetic insights from combining isolated population and national health register data. medRxiv. 2022:2022.03.03.22271360.
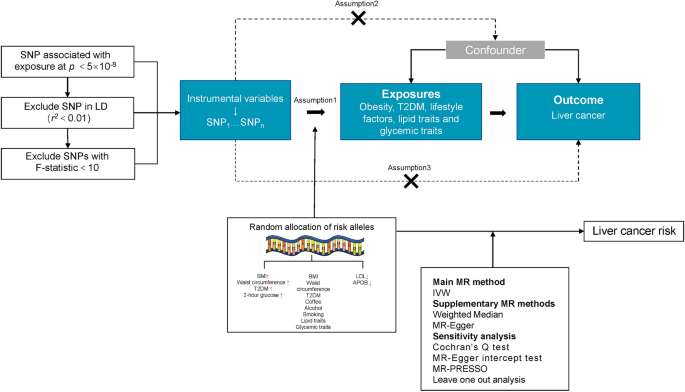
Burgess, S. et al. Guidelines for performing Mendelian randomization investigations [version 2; peer review: 2 approved]. Wellcome Open Res. 4, 186 (2020).
Google Scholar
Papadimitriou, N. et al. Physical activity and risks of breast and colorectal cancer: A Mendelian randomisation analysis. Nat. Commun. 11(1), 597 (2020).
Google Scholar
Bowden, J., Davey Smith, G., Haycock, P. C. & Burgess, S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40(4), 304–314 (2016).
Google Scholar
Bowden, J., Davey Smith, G. & Burgess, S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 44(2), 512–525 (2015).
Google Scholar
Rees, J. M. B., Wood, A. M. & Burgess, S. Extending the MR-Egger method for multivariable Mendelian randomization to correct for both measured and unmeasured pleiotropy. Stat. Med. 36(29), 4705–4718 (2017).
Google Scholar
Hemani, G., Zheng, J., Elsworth, B., Wade, K. H., Haberland, V., Baird, D. et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 7 (2018).
Lin, Z., Deng, Y. & Pan, W. Combining the strengths of inverse-variance weighting and Egger regression in Mendelian randomization using a mixture of regressions model. PLoS Genet. 17(11), e1009922 (2021).
Google Scholar
Yuan, S., Gill, D., Giovannucci, E. L. & Larsson, S. C. Obesity, type 2 diabetes, lifestyle factors, and risk of gallstone disease: A Mendelian randomization investigation. Clin. Gastroenterol. Hepatol. 20(3), e529–e537 (2022).
Google Scholar
Bowden, J. et al. Assessing the suitability of summary data for two-sample Mendelian randomization analyses using MR-Egger regression: The role of the I2 statistic. Int. J. Epidemiol. 45(6), 1961–1974 (2016).
Google Scholar
Yuan, S. & Larsson, S. C. Adiposity, diabetes, lifestyle factors and risk of gastroesophageal reflux disease: A Mendelian randomization study. Eur. J. Epidemiol. 37(7), 747–754 (2022).
Google Scholar
Chen, X. et al. Causal relationship between physical activity, leisure sedentary behaviors and COVID-19 risk: A Mendelian randomization study. J. Transl. Med. 20(1), 216 (2022).
Google Scholar
Pierce, B. L., Ahsan, H. & VanderWeele, T. J. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int. J. Epidemiol. 40(3), 740–752 (2010).
Google Scholar
Yang, C. et al. Excess body weight and the risk of liver cancer: Systematic review and a meta-analysis of cohort studies. Nutr. Cancer. 72(7), 1085–1097 (2020).
Google Scholar
Florio, A. A. et al. Abdominal and gluteofemoral size and risk of liver cancer: The liver cancer pooling project. Int. J. Cancer. 147(3), 675–685 (2020).
Google Scholar
Rahmani, J. et al. Waist circumference and risk of liver cancer: A systematic review and meta-analysis of over 2 million cohort study participants. Liver Cancer. 9(1), 6–14 (2020).
Google Scholar
De Lorenzo, A. et al. Normal-weight obese syndrome: Early inflammation?. Am. J. Clin. Nutr. 85(1), 40–45 (2007).
Google Scholar
Fasshauer, M. & Blüher, M. Adipokines in health and disease. Trends Pharmacol. Sci. 36(7), 461–470 (2015).
Google Scholar
Catalán, V., Gómez-Ambrosi, J., Rodríguez, A. & Frühbeck, G. Adipose tissue immunity and cancer. Front. Physiol. 4, 275 (2013).
Google Scholar
Zhang, C., Liu, S. & Yang, M. Hepatocellular carcinoma and obesity, type 2 diabetes mellitus, cardiovascular disease: Causing factors, molecular links, and treatment options. Front. Endocrinol. (Lausanne). 12, 808526 (2021).
Google Scholar
Davila, J. A., Morgan, R. O., Shaib, Y., McGlynn, K. A. & El-Serag, H. B. Diabetes increases the risk of hepatocellular carcinoma in the United States: A population based case control study. Gut. 54(4), 533–539 (2005).
Google Scholar
Schlesinger, S. et al. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: Umbrella review of meta-analyses of prospective studies. Diabetologia. 65(2), 275–285 (2022).
Google Scholar
Rapp, K. et al. Fasting blood glucose and cancer risk in a cohort of more than 140,000 adults in Austria. Diabetologia. 49(5), 945–952 (2006).
Google Scholar
Sakurai, Y. et al. Role of insulin receptor substrates in the progression of hepatocellular carcinoma. Sci. Rep. 7(1), 5387 (2017).
Google Scholar
Hamouda, H. A., Mansour, S. M. & Elyamany, M. F. Vitamin D combined with pioglitazone mitigates type-2 diabetes-induced hepatic injury through targeting inflammation, apoptosis, and oxidative stress. Inflammation. 45(1), 156–171 (2022).
Google Scholar
Gurung, M. et al. Role of gut microbiota in type 2 diabetes pathophysiology. EBioMedicine. 51, 102590 (2020).
Google Scholar
Kawaguchi, T. et al. Spontaneous regression of hepatocellular carcinoma with reduction in angiogenesis-related cytokines after treatment with sodium-glucose cotransporter 2 inhibitor in a cirrhotic patient with diabetes mellitus. Hepatol. Res. 49(4), 479–486 (2019).
Google Scholar
Rao Kondapally Seshasai, S. et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 364(9), 829–841 (2011).
Google Scholar
Hedong Han, T. Z. et al. Blood glucose concentration and risk of liver cancer: Systematic review and meta-analysis of prospective studies. Oncotarget. 8(30), 50164–50173 (2017).
Google Scholar
Zhengming Chen, A. K. et al. Prolonged infection with hepatitis B virus and association between low blood cholesterol concentration and liver cancer. BMJ (Clin. Res. Ed.) 306, 890–894 (1993).
Google Scholar
Borgquist, S. et al. Apolipoproteins, lipids and risk of cancer. Int. J. Cancer. 138(11), 2648–2656 (2016).
Google Scholar
Benn, M., Tybjaerg-Hansen, A., Stender, S., Frikke-Schmidt, R. & Nordestgaard, B. G. Low-density lipoprotein cholesterol and the risk of cancer: A mendelian randomization study. J. Natl. Cancer Inst. 103(6), 508–519 (2011).
Google Scholar
Lee, G. et al. Clinical significance of APOB inactivation in hepatocellular carcinoma. Exp. Mol. Med. 50(11), 1–12 (2018).
Google Scholar
Comprehensive and integrative genomic characterization of hepatocellular carcinoma. Cell. 169(7), 1327–41.e23 (2017).
Cho, Y. et al. Association between lipid profiles and the incidence of hepatocellular carcinoma: A nationwide population-based study. Cancers (Basel). 13(7), 1599 (2021).
Google Scholar
Mao, X. et al. Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: New findings and future perspectives. Mol. Cancer. 20(1), 131 (2021).
Google Scholar
Qin, W. H. et al. High serum levels of cholesterol increase antitumor functions of nature killer cells and reduce growth of liver tumors in mice. Gastroenterology. 158(6), 1713–1727 (2020).
Google Scholar
Bagnardi, V. et al. Light alcohol drinking and cancer: A meta-analysis. Ann. Oncol. 24(2), 301–308 (2013).
Google Scholar
Chuang, S. C., Lee, Y. C., Wu, G. J., Straif, K. & Hashibe, M. Alcohol consumption and liver cancer risk: A meta-analysis. Cancer Causes Control. 26(9), 1205–1231 (2015).
Google Scholar
Turati, F. et al. Alcohol and liver cancer: A systematic review and meta-analysis of prospective studies. Ann. Oncol. 25(8), 1526–1535 (2014).
Google Scholar
Kennedy, O. J. et al. Coffee, including caffeinated and decaffeinated coffee, and the risk of hepatocellular carcinoma: A systematic review and dose-response meta-analysis. BMJ Open. 7(5), e013739 (2017).
Google Scholar
Davies, N. M., Holmes, M. V. & Davey, S. G. Reading Mendelian randomisation studies: A guide, glossary, and checklist for clinicians. BMJ (Clin. Res. Ed). 362, k601 (2018).
Google Scholar
Holmes, M. V., Ala-Korpela, M. & Smith, G. D. Mendelian randomization in cardiometabolic disease: Challenges in evaluating causality. Nat. Rev. Cardiol. 14(10), 577–590 (2017).
Google Scholar