BOSTON — Gov. Maura Healey on Thursday cited “changes in circumstances” at financially challenged Steward Healthcare, which operates nine hospitals in Massachusetts, in an effort to ensure stability for the state's health care system. He said he is focusing on.
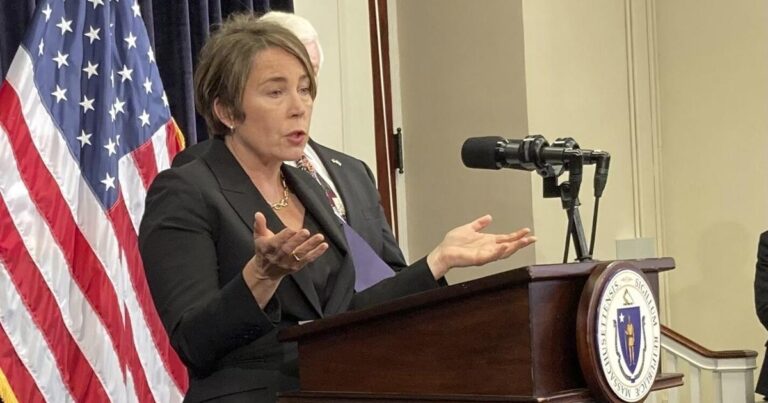
“Our first job is to protect patients, protect access to health care, and protect and stabilize our health care system,” Healy told reporters after the event in Newton. “So that's what we're focused on. (Health and Human Services) Secretary (Kate) Walsh and her team and our administration are working closely with everyone involved in this. We are continuing to communicate. It is an evolving situation. But our job is to protect patients, access to care, and the stability of our health care system.”
Attorney General Andrea Campbell also said she was prepared to act if necessary.
“Our priority now is to protect patients, access to health care and the jobs of those who make that care possible,” Campbell said in a statement Thursday. “While we are currently in problem-solving mode and are willing to use every power available to us to protect these priorities, it is time for Steward to seriously address why we found ourselves in this situation in the near future.” We are looking forward to.”
On Tuesday, members of the Massachusetts congressional delegation sent a letter to Ralph de la Torre, CEO of Dallas-based Steward, stating that any of Steward's hospitals in Massachusetts would close. The patient was reminded of the serious consequences if this happens.
Stewards will be attending Holy Family Hospitals in Haverhill and Methuen, Carney Hospital in Dorchester, Good Samaritan Medical Center in Brockton, Morton Hospital in Taunton, New England Air's Nashoba Valley Medical Center, and Sinai Hospital in Stoughton. It operates a hospital, Norwood Hospital (closed after the accident and under construction). flood), St. Ann's Hospital in Fall River, and St. Elizabeth Medical Center in Brighton.
The company employs more than 16,000 nurses, doctors and other health care workers in Massachusetts, according to representatives.
In the letter, the delegation cited a Jan. 19 Boston Globe report showing Steward was in “severe financial distress,” the company's plans to close New England Sinai Hospital, unpaid rent and Medical Property Trust's Jan. 4 report on loan payments charges Steward St. Elizabeth Medical Center, Steward Medical Group, and Steward Healthcare System with federal charges of violating the False Claims Act. The government filed a complaint.
The delegation also requested a financial briefing from the stewards, which the stewards agreed to.
“This shows how important our community hospitals are to our state,” company spokeswoman Deborah Chiarabaroti said in an email to the News Service Thursday. “Seventy percent of our patients are covered by state and federally funded programs, so I look forward to briefing the delegation and exploring potential solutions.”
Hospital systems across Massachusetts are strained by a combination of patient demand, workforce constraints, and funding challenges. On January 9, Secretary Walsh outlined an agreement between hospitals, nursing homes, insurance companies, and state regulators to voluntarily and temporarily change operations to alleviate strained patient capacity. . Lawmakers across the state are closely monitoring the situation at Steward and at hospitals other than Steward, keeping in mind the impact on their constituencies and the possibility of interference.
Asked Wednesday about the Senate's role in responding to Steward, Senate President Karen Spilka said, “Do you have about four hours left?”
“This is a very complex issue and it's evolving every day,” Spilka said. “So we are working closely with the administration to monitor and find out what is happening with different hospitals in this situation.”
“It's too early to say at this point,” Spilka said when asked if government officials were evaluating possible national receivership or legislative options.
Real estate investment trust Medical Properties Trust earlier this month cited Steward's delayed and partial rent payments and said Steward's “liquidity has been adversely affected by significant changes to vendor payment terms.” He said he was informed by the company.
MPT said the team will work closely with Steward, which operates 33 community hospitals in nine states, and that “if successful, it will strengthen Steward's liquidity to restore its balance sheet and MPT's ability to recover unpaid rent.” “A plan of action aimed at optimizing the Ultimately he will be less exposed to MPT stewards. ”
MPT said that as part of its action plan, Steward is pursuing “several strategic transactions, including the potential sale or re-tenancy of certain hospital operations and the sale of non-core operations.” .
The company is also focused on finding a capital partner for its managed care business, the proceeds of which will be used to repay a portion of the outstanding debt to MPT, and Steward also said it would “establish a transformation committee.” MPT and its ABL lenders are comprised of newly appointed independent directors who have strengthened measures to improve recovery and overall governance, including providing regular cash activity and asset sale progress reports to MPT and its ABL lenders. ,” MPT said.
In Newton, a reporter asked Healy about the role of the state's two largest hospital groups, Massachusetts General Brigham and Beth Israel Lahey Health.
“As far as what they are proposing, we haven't seen the plans from the stewards yet so I won't comment until they are clear, but that's what we're monitoring very closely. We know that,” Healy said. He said.
According to Steward, the company is working to “strengthen its liquidity, restore its balance sheet, and put in place the tools necessary to continue moving forward as a leading provider of health care services to our patients, communities, physicians, and employees.” We are proceeding with an action plan.”
In 2010, after a five-month review of a proposed deal between Steward and the faith-based Caritas Health System, Attorney General Martha Coakley conditionally approved a proposed deal between Brighton, Brockton, Dorchester and Methuen. Supported the plan to transfer the hospital. , Norwood and Fall River to Steward for $495 million.
In a report submitted by Mr. Coakley at the time, the Attorney General's Office concluded: Risk of not trading. Additionally, the additional protections and transparency obtained by the Attorney General will ensure that the system remains a system, avoids the closure of Caritas Hospital, funds pension obligations, repays debt, and addresses deferred funding needs. It has the advantage of starting the process. Caritas is clear and convincing. ”
In a statement Thursday, Steward cited its founding mission in 2010 to “provide quality care to the most marginalized patient populations,” and how it will “absorb the failing Caritas Christi Regional Hospital system.” “He worked with a unique attitude to achieve this goal.''
The company said it faces growing disparities between commercial reimbursement to large academic medical centers and payments to Steward's community hospitals in Massachusetts, which serve large numbers of Medicare and Medicaid patients. Ta.
“This gap is only widening, and most community hospitals, including Steward Hospital in Massachusetts, are suffering losses that jeopardize their ability to continue providing services,” Steward said.
Additionally, “Steward Healthcare is one of many health systems in Massachusetts that previously faced severe, long-tail impacts from the COVID-19 pandemic. Record losses, The state's community hospitals have been devastated over the past few years, with significant downsizing and facility closures.”
The company also cited community hospitals and advocacy for reform of medical fee disparities during the government administration. Deval Patrick and Charlie Baker said they were continuing to hold discussions with Healy and Campbell.