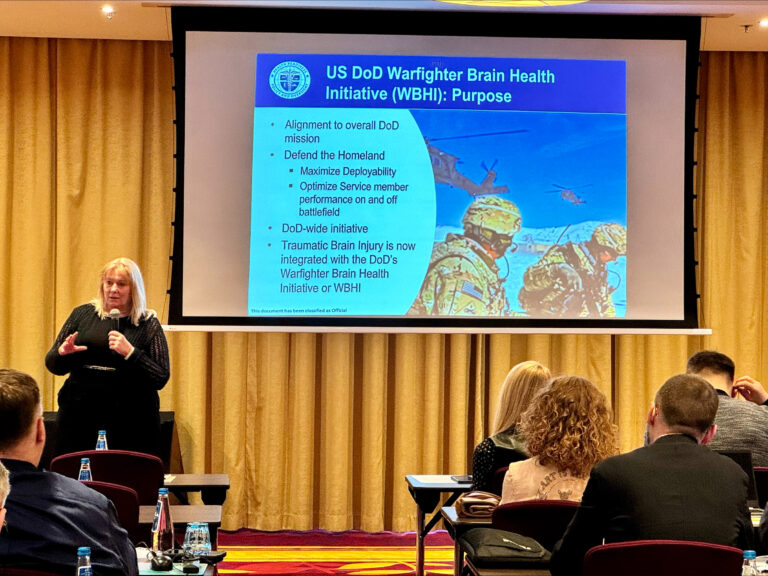
Kathie Lee, Department of Defense policy director for warfighter brain health, speaks about traumatic brain injury and military intelligence at the U.S.-Ukrainian Medical Symposium on Brain Health in Poland on March 15, 2024. He gave a talk on preparedness.
This symposium was dedicated to addressing the comprehensive area of brain health, including both traumatic brain injury and mental health challenges. The aim is to assess brain health in the context of the Ukraine war, identify critical issues affecting patient outcomes, develop integrated brain health strategies for improvement, and advance international research in brain health science. The aim was to strengthen cooperation.
The Department of Defense defines U.S. warfighter brain health as the physical, psychological, and cognitive conditions that impact a warfighter's ability to function adaptively in any environment, improving readiness, operational ability, and mission. effectiveness and the goal of achieving overwhelming or superior lethality.
Mr. Lee discussed treatment pathways for traumatic brain injury in the field and in military hospitals and clinics. These include:
- Standardization of clinical tools and clinical recommendations
- Conduct comprehensive education and training activities for all key stakeholders
- Establish and enforce policies to ensure compliance and maintain oversight
- Applying research results to the field to further improve care
Since 2000, 492,167 military personnel have been diagnosed with traumatic brain injury, Lee said. Of these, 82.2% were considered mild, followed by 11.4% moderate, 1% severe, and 1.2% penetrant (4.2% unclassifiable). The military medical system sees an estimated 14,000 to 17,000 visits a month for traumatic brain injuries, with the majority coming from active-duty military personnel, she said. Additionally, 15 to 30 percent of active-duty military members experience long-term symptoms from traumatic brain injury.
Mild traumatic brain injury at the scene
In his second presentation, Lee highlighted lessons from the field regarding mild traumatic brain injuries, commonly known as concussions.
Lee told the audience that the Pentagon is “widely aware of the events that can lead to concussions and mild traumatic brain injuries” in combat settings.
Examples of occupational hazards include heavy weapons fires, missile and tank fires, and training and breach exercises where military personnel and their instructors may be exposed to explosive overpressure. Blast overpressure is the “wave” you feel after firing a weapon or ammunition. When explosive overpressure waves occur, they can affect thinking skills, balance changes, and other brain health issues.
Warfighters who are in a deployed environment and are exposed to events that can cause a concussion, even if exposed to a single blast, are subject to mandatory medical evaluation and 24-hour monitoring, rest, and A report is required, Lee said.
Required medical evaluation criteria include:
- Involvement in vehicle explosions, collisions, or rollovers
- Presence within 50 meters of explosion (indoors or outdoors)
- Witnessing a direct blow to the head or loss of consciousness
- If a commander is exposed to multiple explosive incidents while directing a medical evaluation
Mr. Lee also discussed concussion screening using the MACE 2 field assessment tool and the required neurological evaluation, which tests overall sensory and motor function. These evaluations include:
- fluency of speech
- word search
- grip strength
- pronator drift
- standing on one leg
- tandem walking
- pupil reaction
- eye tracking
The symposium audience also heard about vestibulo-oculomotor screening techniques, the constellation of symptoms that may appear after mild traumatic brain injury, and the progressive stages of return to activity and return to duty.
Overall, the bilateral exchange is working to advance brain injury treatment protocols, support expansion of treatment capacity and patient transport, and modernize screening processes, training, and treatment practices.
“This symposium was a unique and valuable opportunity to share lessons learned from the critical brain health area that impacts the readiness and performance of Ukrainian and U.S. warfighters,” Lee said.
WBHI will be codified as a program in the summer of 2022 and continues its mission to assess, monitor, and minimize risk, understand the effects of traumatic brain injury, and improve warfighter performance and readiness. Masu.