Walter Berkehiser, 52, of Denton, North Carolina, loves riding motorcycles and four-wheelers. He enjoys spending time outdoors and gardening. Walter retired from the Marine Corps after 24 years of service. He frequently volunteers to help homeless veterans and supports charity fundraisers benefiting veterans.
A few years ago, Walter was driving down Highway 64 around 10 a.m. when he felt dizzy so he pulled over to the side of the road, where the driveway was only 4 inches wide. As he waited until the car approached the driveway, he lost consciousness and rolled his truck to the side of the road.
Walter woke up quickly and was fortunate enough to be able to leave the accident scene unharmed. An ambulance came and took him to a local hospital, where the care team placed him on an electrocardiogram machine. His doctors attributed this event to fatigue and perhaps hunger. He was released that night.
A few months later, Walter was diagnosed with high blood pressure and was put on medication to control his blood pressure. One of the side effects of the drug is a severe headache, but he has learned how to cope with it.
A year after his first accident, Walter loses consciousness while driving and crashes his car into a ditch. When he woke up, he found himself upside down in the car. Paramedics rescued him and took him to hospital for further tests.
Hospital staff discovered two blockages in his heart. He inserted two stents to keep the artery open. He also had a blockage in his left anterior descending artery, also known as the Widowmaker's artery. They decided to keep an eye on the widow's artery for now.
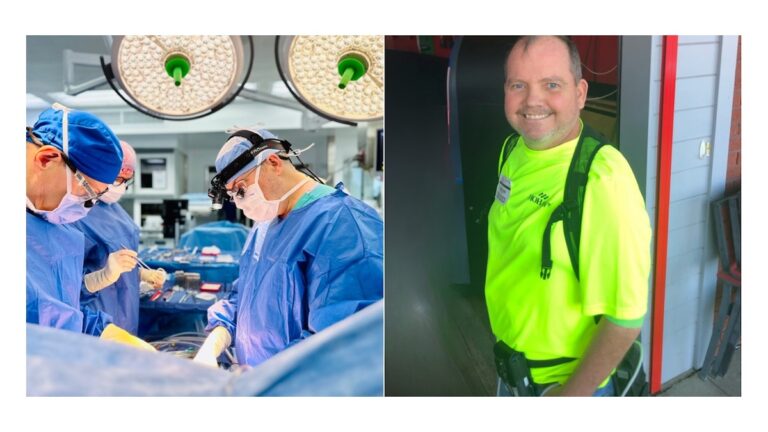
In December 2022, Walter felt unwell and returned home from work. He asked his neighbor to take him to the emergency department. Staff discovered that Walter was in the midst of a heart attack. Within 10 minutes of arriving, they sent him to Atrium Health Wake Forest He Baptist, where Wake Forest He was a cardiothoracic surgeon and professor of surgery at Baptist, Bart He Imielski, Ph.D. It was evaluated by
Dr. Imierski pinpointed the cause of Walter's power outages as chronic blood flow problems caused by advanced coronary artery disease. Walter's heart was not suitable for bypass surgery as he was only functioning at 15%.
temporary cardiac support
Imielski suggested an impeller.® heart pump. By temporarily supporting the pump function, the heart can rest. Wake Forest Baptist recently installed its 100th Impeller, marking a significant milestone in its advanced heart failure and transplant programs. This collaborative program of heart failure cardiologists and surgeons produces the best heart transplant outcomes in North Carolina.
“Our program is in the top 25% in the country for Impella utilization,” Imielski explains. “This device helps support patients with low cardiac output, stabilizes patients with heart failure, and strengthens them for heart surgery or left ventricular assist devices (LVADs).”
Walter required extracorporeal membrane oxygenation (ECMO) therapy because of the difficult early course of his illness. This treatment involves pumping the patient's blood through an artificial circuit. The immediate danger to his life was finally stabilized.
Walter was in such critical condition that Impella and ECMO therapy were used to save his life, giving his organs time to recover and his body regaining strength before undergoing further treatment. . After several weeks of applying these treatments, Walter remained in heart failure.
artificial heart pump
Dr. Imierski recommended an LVAD, which functions like a water pump, to support Walter's heart while he waits for a transplant. It is attached to each end of the heart and continuously pumps blood. Imielski also tracks Walter's heart activity for monthly review.
There is a wire on the side of the pump that exits from an area near Walter's stomach and connects to an external controller about the size of a large TV remote. Walter wears a harness with a battery pack to power the device. The pack weighs about 8 pounds and will last from 6 and a half hours to 8 hours after a full charge. At bedtime, Walter connects her LVAD to her 30-foot cord that connects to an external battery pack.
Before taking a shower, Walter must ensure that all wire connections are watertight to prevent damage. With an LVAD, Walter is unable to swim or soak in a bathtub or hot tub.
exceptional care and encouragement
Walter's care team at Wake Forest Baptist provided excellent care 24/7.
“They went above and beyond for me and always made me feel like I was part of their family,” Walter says. “I always felt comfortable asking questions about my care and treatment.”
Walter also appreciated the positivity of his care team, which helped him battle depression during his recovery.
“They always encouraged me to stay active, which made me stronger,” Walter says. “They were always joking and always smiling. That made the difference for me.”
Walter's nursing team took care of every detail, no matter how small. When his back was itchy, a nurse scratched his back. The next day, the nurse brought Walter a scratcher for his back.
learn and support others
It took Walter several months to recover and regain his strength. But now he feels better and can enjoy many of his favorite activities while waiting for his transplant. Thanks to the LVAD, he is excited about his newfound freedom to walk, drive, and ride his motorcycle.
Walter is still learning how to use and test LVADs. He has a daily checklist to check its functionality. If he notices any numbers that seem unusual, he calls Imielski's office and heads to the hospital.
Mr. Walter is happy to work with Wake Forest Baptist's LVAD coordinator to help support patients considering this unique heart pump.
“I tell them about my experience and the additional equipment they have to carry,” says Walter. “But I also explain how much better I feel now that my blood is pumping properly. I try to be positive and encouraging while being realistic about the challenges.”
For more information, Advanced Heart Failure and Transplant Program at Atrium Health Wake Forest Baptist.