And it's surprisingly easy.
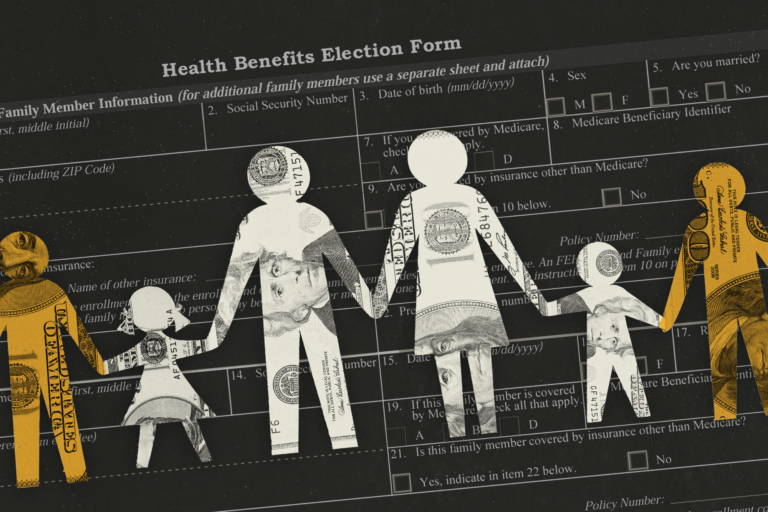
The Office of Personnel Management, which oversees health insurance for 8 million federal employees and their families at a cost of more than $60 billion a year, is responsible for the They say they have never checked their qualifications. The company has been asking OPM to improve its oversight for years. And that failure is costing taxpayers billions of dollars and raising insurance premiums for millions of public employees.
That is unacceptable, the senator said. rick scott (R-Fla.) plans to introduce a bill in March that would require OPM to audit its members.
“OPM doesn't care about cheating. Otherwise they would cheat. It's not that hard,” said Scott, who requested the GAO report. “Companies do it all the time, and states do it all the time. It's very easy to put programs in place to do it, so if you don't do it, you're supporting fraud.” It will be.”
An OPM spokesperson balked at claims that fraud is not a high priority, telling Politico that OPM is “acting in good faith.” [Federal Employees Health Benefits] We take our program very seriously and are working diligently with government agencies to address inappropriate registrations within the constraints of resources from Congress. ”
Despite efforts from GAO, the agency has no plans to conduct an audit, saying it would be too expensive. The agency enrolls and verifies eligibility for members of the Federal Employees Health Benefits Program under more than 70 contracts with more than 160 government employment agencies and health insurance companies.
According to OPM, this means the $120 million audit will be expended from OPM's budget, with the savings accruing to registered agents.
“This is not an easy problem to solve, there's no question about that,” said Assistant Auditor General Michael Esser, who oversees audits of all OPM-managed programs. “But this can become a very costly problem if not addressed.”
Mr. Esser's office estimates that ineligible enrollees cost federal health programs between $250 million and $3 billion a year, and the lack of accounting for improper payments is a sign of OPM's “This is a persistent issue for top management.”
“OPM passivity”
OPM may claim that addressing inadequacies is a priority, but “they never act like that,” according to GAO Forensic Audits and Investigations, which authored the 2022 report. said Seth Bagdoyan, director of the service team. Bagdoyan said Congressional action may be the only way to force OPM to address the issue.
“We found that OPM was passive in its oversight role, so we essentially concluded that program integrity and risk management were not clear priorities for OPM,” Bagdoyan said.
Mr. Scott's bill would not provide new funding to OPM, but would require it to remove ineligible members from the program, evaluate the likelihood and impact of misconduct, and document that evaluation, among other things. It mandates implementation of GAO's recommendations.
The Florida senator is confident this bill will garner bipartisan support.
“I don't think anyone would object to that unless they were going to run a campaign saying they liked fraud,” he says.
Scott conducted an audit of the state's health benefits plan when he was Florida's governor, which found that about 3 percent of enrollees were ineligible, resulting in the state losing $20 million a year. I ended up saving more than a dollar.
At least 25 states have conducted audits of their benefit programs, according to GAO. New Jersey saved taxpayers tens of millions of dollars after a 2019 audit removed more than 13,000 ineligible dependents from the state's health care plan.
In California, a multi-year project to verify eligibility for the State Public Employees' Retirement System's health insurance plan resulted in the removal of 2.6 percent of dependents in 2015, costing the state approximately $122 million during the audit period. Saved money.
And all 50 states have reviewed eligibility for all Medicaid recipients over the past year for the first time since the end of the coronavirus public health emergency, with at least 17 million people having lost their insurance to date, according to the KFF Tracker. It is said that he will lose his. .
OPM has no plans to conduct an audit, but a spokesperson said the agency has launched a new FEHB Master Registration Index. This is a list of all federal employees and their families enrolled in the program that the agency can use to more easily identify ineligible enrollees. Removal. ”
The spokesperson also said the agency is “training agencies and health care providers on enrollment verification and implementing centralized enrollment for all new benefit programs offered to federal employees since 2000.” OPM is developing a centralized enrollment system for the new Postal Service Health Benefits Program, a separate initiative within FEHB for postal employees, a spokesperson said.
FEHB registration verification and tracking is primarily decentralized and left to federal agencies rather than OPM. OPM's “clear path forward” is not to conduct retrospective audits, but rather “a fully FEHB-funded, centralized registration system that addresses the underlying issues of inadequate registration.” Yes, the spokesperson said.
OPM declined to comment on whether it is pursuing funding for a centralized registration system or the status of the system's implementation.
“We continue to work with Congress to modernize and improve the FEHB program to better serve federal employees and their families,” the spokesperson said.
“Potential size”
GAO, which conducted the audit from May 2021 to December 2022, interviewed five government agencies and the program's five health insurers, which routinely identify ineligible families. and reported that no exclusions were made.
The employing office or carrier may only discover that a member is no longer eligible if the employee changes coverage or is tipped off by the employee.
In January 2017, a federal agent was arrested in this manner. A health insurance company discovered that when a subscriber added his new wife to the plan, he submitted falsified court documents to exclude his ex-wife from the plan. Documents show he divorced his ex-wife in 2017, with the actual divorce taking place in 1993. The government paid more than $150,000 in claims on behalf of his ex-wife for 14 years of ineligible coverage.
In another example, the agency's Office of Inspector General used federal employees to keep their children on health insurance past their 26th birthday, even though they were not capable of supporting themselves. I received hotline information stating that I was registered as a dependent without a child. Be independent and not qualify for a disability. The government paid out more than $160,000 in improper payments, including claims from multiple drug rehabilitation centers.
Through a tip from another hotline, OIG discovered that a former Federal Highway Administration employee had sought insurance coverage for his sister and niece for 12 years by claiming they were his wife and stepchildren. . The government spent more than $100,000 in premiums and reimbursements for the two ineligible members.
The GAO report notes that OPM does not have accurate estimates of how many members are ineligible for the program. But that number could be in the thousands, based on an audit of state health plans.
There are varying estimates of the cost of the program for ineligible enrollees. The GAO report estimates the cost at $1 billion per year, but that number is based on information from OPM and is a “very rough indication of the potential scale of fraud” in the program. '' Bagdoyan said. That number could be even higher, he said, considering the tens of millions of dollars in savings states realize as they conduct audits of their health plans.
Since the inception of the Federal Employee Health Benefits Program in 1960, OPM has screened documents confirming family eligibility for new hires, life event eligibility, or open season enrollment at the employer's office. I never asked for it. The agency updated its guidance in April 2021 to require offices to verify family eligibility for new hires and qualifying life events, but not during open recruitment periods.
However, GAO's report found that not all offices followed OPM's guidance for new enrollees and did not regularly monitor the eligibility of currently enrolled families.
The new guidance also did not address people who may have been fraudulently enrolled in the program. Additionally, OPM does not monitor whether employer offices or carriers are complying with the agency's guidance on eligibility verification.
“It just reinforces the negative idea that, 'Well, everyone else is to blame,' and we're not really responsible,” said Bagdoyan, author of the GAO report. . “That's what we've learned over the past few years working on this issue.”
And Chris Deacon, former deputy director of the New Jersey Department of Pension Benefits, who helped oversee the state audit in 2019, said that managing health care costs, especially in light of the jump in workplace insurance premiums in 2023, will The Lord said it was something he should pay more attention to.
As the largest self-funded health plan administrator in the United States, OPM sets an example for other large employers across the country, rather than taking a hands-off approach or relying on vendors and contractors. have a chance. The provider has the power to decide,” Deacon said. Instead, the agency has taken a “slightly territorial” and “defensive attitude” toward discovering fraud, waste and abuse within the program, she added.
“They are dealing with taxpayers' money, and their trust and fiduciary duty to spend that money wisely and prudently is certainly greater than what employers have to do. '' Deacon said. “So it would be a missed opportunity for them not to take a leading role in how health insurance is purchased more prudently and in a way that benefits plans and plan members.”