I just wanted to solve the mystery of why I wake up tired, and it’s led me to this moment: Electrodes glued to my scalp and face, to read every twitch, eye roll and brainwave as I sleep. Wires stretching down to a glowing control box strapped to my waist. A flow sensor in my nostrils to measure my breathing.
This isn’t how I normally go to bed.
I’m at Stanford’s Sleep Medicine Center for a polysomnography, the gold standard method for diagnosing sleep disorders. Jonathan Campbell, a friendly sleep technician, has just spent 45 minutes gluing and strapping equipment to my body. He’ll monitor me overnight from the control room, watching my brain activity, heart rate and body movement and listening for snoring in real time.
He’s been doing this for 20 years. “It boggles my mind. To this day I still get some adults asking me, ‘Can you see my dreams?'” he says, applying blobs of adhesive to my forehead with a Q-tip.
I’m not alone in having trouble sleeping. According to the National Heart, Lung and Blood Institute, between 50 million and 70 million Americans have sleep disorders, and one in three adults don’t get the recommended amount of uninterrupted sleep they need. People sleep badly for so many different reasons: stress, chronic pain, environmental factors like noise — the list goes on. Getting less than the recommended amount of sleep is a slippery slope to a variety of health issues, and we all know how it can make us feel like a walking dumpster fire the next day.
You might already track your sleep using an Apple Watch, Fitbit, Galaxy Watch or similar wearable and have a general idea of how you sleep. These trackers can give more insight into the amount of time we spend in different sleep stages like rapid eye movement (REM) or deep sleep and may help identify areas we can improve through lifestyle tweaks. But they can’t diagnose sleep disorders — yet.
That’s where a lab-based sleep test comes in, though home sleep tests are also an option. Over 80 clinical sleep disorders can be identified during a sleep test, including insomnia, narcolepsy and sleep apnea, a condition in which you stop breathing momentarily. But if you don’t suspect a sleep disorder and want to try to improve your rest, there’s a plethora of weird and wild sleep tech that promises to do just that.
Smart sleep masks like the Aura Circle block out external light during the evening and simulate sunrise to gently wake you up. Neurofeedback headsets like the Sens.ai claim to analyze and train your brainwaves so you get better sleep. Hastens, the oldest bed maker in the world, has a luxurious horse-hair mattress called Grand Vividus that costs almost $400,000. There’s even a soft, peanut-shaped sleep robot, the Somnox 2, for cuddling in bed to regulate your breathing. (I tried the original Somnox while reporting from the CES trade show in 2018, and it helped me drift off during a particularly stressful week.)
The “sleep economy” — beds, mattresses, sleep aids and medical equipment — is estimated to be worth almost $600 billion this year. But how do you know what really works without spending an absolute fortune on trial and error? One way is to check product reviews: CNET’s team of experts, for instance, has reviewed more than 200 mattresses and other products at a lab in Reno, Nevada.
Or, if you’re like me, you conduct your own personal sleep experiment.
This took place over the better part of a month. The first week was about getting my sleep habits in order, adjusting my wakeup time and integrating some inexpensive sleep tools like a weighted blanket. In week two, I tested gadgets designed to promote sleep, including the $199 Therabody SmartGoggles with heated massage, and guided meditations from Centr, a fitness and wellbeing app ($30 a month, or $120 for a full year). Then for week three, the budget went out the window. I tried a $2,500 infrared sauna from Clearlight and the similarly priced Eight Sleep Pod 3 (the top-of-the-line model), a heating and cooling system for your mattress.
Throughout the three weeks, I tracked my sleep each night with the $299 Oura Ring 3 because it’s more comfortable for me to wear in bed than a smartwatch. It also gives a sleep score out of 100, helpful for tracking my progress over time. In addition, I talked to a range of sleep experts to get the secrets on how we can all improve our sleep and to learn the pitfalls when it comes to tracking our rest.
At the end of that stretch, I did the Stanford sleep lab test to get a full-on scientific assessment of my sleep and insights into what might be keeping me from getting a perfect night’s rest.
Read on to see how I fared each week, what I’ve learned from the whole experience and how it could help you with your own slumbers.
Meeting the sleep doctor
At the Sleep Medicine Center I get my first look at the bedroom where I’ll spend the night. Over the bed is an infrared camera, and a cupboard to one side is filled with control boxes. It feels like a cross between a laboratory and a hotel room. The window looks out over a freeway, but I can’t hear a thing thanks to four layers of glass. The bed is very comfortable.
“Amazingly, people can always sleep [in here] eventually,” says Dr. Rafael Pelayo.
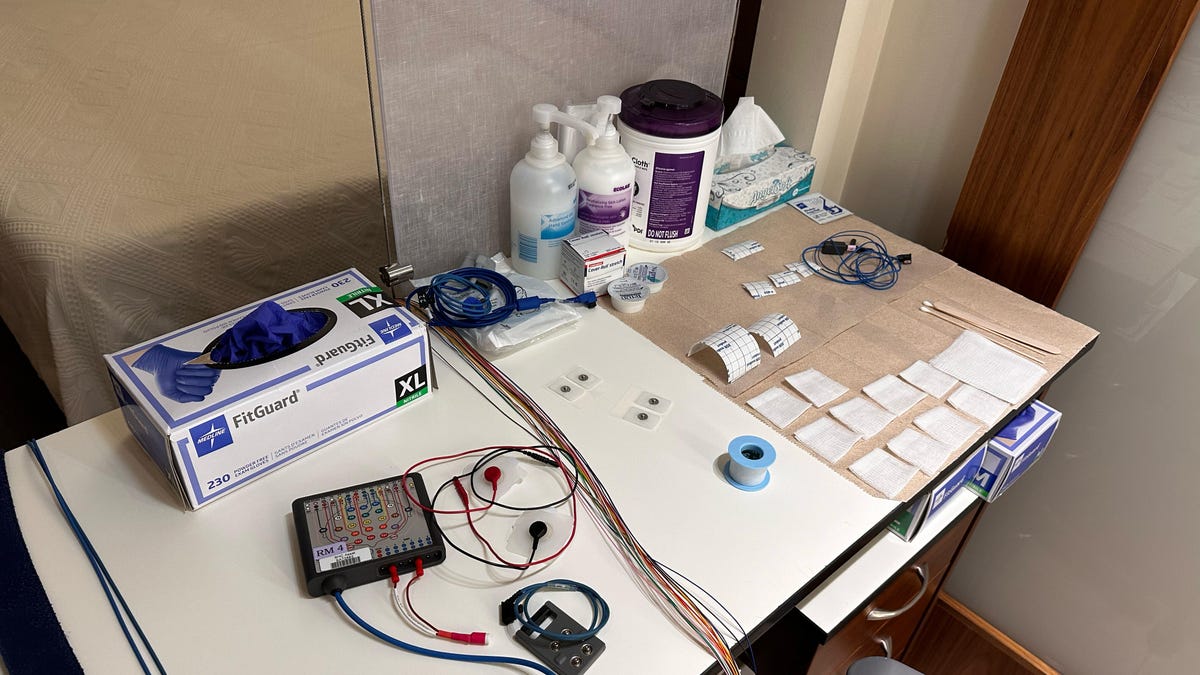
Electrodes, control boxes and adhesive are all laid out on a table for the sleep technician.
Pelayo is a clinical professor at Stanford University in California and one of the most renowned doctors in the world working in sleep medicine. We wind our way to his office, making a stop to see an early homemade CPAP machine used to treat sleep apnea. It looks like an air compressor and sounds like a vacuum cleaner, and Pelayo tells me he did his one and only dumpster dive to rescue it when it was about to get thrown out.
His office is filled with sleep-related ephemera including a topsy-turvy Little Red Riding Hood toy. When you flip it upside down, it morphs into the wolf, dressed as grandma lying in bed and waiting to pounce on the heroine.
Lining the wall is a collection of custom-printed T-shirts with slogans like “I Sleep, Therefore I REM” and “Drowsiness is Red Alert.” That’s the motto students need to shout if they fall asleep during Pelayo’s class, Dement’s Sleep and Dreams, accompanied by a squirt of water to wake them up. Studying sleep is anything but boring.
“People sometimes overlook the fact that sleeping is something you learn how to do,” Pelayo says as we talk about my sleep issues, which have been going on for about a year and a half. I noticed my sleep start to change just before I became pregnant. Now I often wake up feeling tired and experience bouts of insomnia for no apparent reason, which I chalk up to new parent exhaustion. But it’s a stark contrast to how I used to sleep.
“The cool thing about this,” Pelayo says, “is once you start sleeping better, once you learn how this works, people keep sleeping better long term.”

William Dement (pictured) is considered the father of sleep medicine. When he retired, he selected Pelayo as his successor to teach his class Sleep and Dreams, the world’s first university course devoted to the science of sleep.
A consultation with a sleep doctor starts with a medical history and physical exam, then examining the actual complaint: Are you struggling to stay awake during the day? Is your spouse or bed partner complaining about snoring? Pelayo says he also wants to know four elements of your sleep: amount, quality, timing and your state of mind. “Just like you can be overweight and malnourished,” he says, the hours of sleep are not as important as the quality of sleep.
Once a doctor decides to do an in-lab sleep test because your sleep quality is in question, there are three parameters to work out if you’re awake or asleep: brainwaves, eye movements and muscle tone. Hence the mess of wires attached to me as I try to fall asleep. There’s also a two-lead electrocardiogram on my chest, motion sensors on my legs and a pulse oximeter on my finger used to track blood oxygen. If it dips lower than 90% during the night, that’s considered harmful and may be a sign of sleep apnea.
It takes me 41.6 minutes to drift off in this new environment. I know the exact time because I’m being monitored to within an inch of my life. When I wake up in the morning, I feel strangely refreshed as I slept over 8 hours undisturbed.
Week 1: The no-tech way to get better sleep
Pelayo gives me a key piece of advice to get my routine in order: lock in a wakeup time, then figure out how many hours of sleep you want and work backward. If your wakeup time depends on when you fall asleep, it throws off your circadian rhythm, the 24-hour clock that tells the body when it’s time to sleep or wake up.
That’s essentially what I’d done in my experiments at home the previous three weeks: Target wakeup time set between 7 a.m. and 7:30 a.m., around the hour my baby rouses. Hopefully, adding a more consistent schedule will get my “sleep hygiene,” or sleep habits, in a good place. My bedroom is already an ideal sleep environment with blackout blinds to block outside light, and I’m pretty good at keeping my phone outside the bedroom. Coffee after lunch? Never! (OK, maybe occasionally.)
Creating a new habit takes time, so I’m giving myself at least seven nights to acclimate to a new routine before making any changes. This week, I’m also trying a range of no-tech sleep tools to go with my new sleep habits. I’ve heard people swear by weighted blankets and I’m trying a $179 12-pound cotton version from Baloo, plus a $159 adjustable body pillow by Twilla. You can add or remove padding, called pods, to your liking.

The Smart Goggles (left) next to the Hatch Restore 2 (right) sitting on top of the Baloo weighted blanket.
The first night I follow Baloo’s advice to start with the weighted blanket only on the lower half of my body so I can acclimate. It’s an interesting sensation and takes a few nights to get used to. Some nights, I wake up from a dream where I’m getting crushed. Maybe the weighted blanket life isn’t for me because it wakes me up when I’m trying to turn in my sleep, even if the blanket itself feels amazing to the touch and looks perfect on my bed.
The body pillow is a bit more my style. I’m primarily a side sleeper, and I like being able to adjust the padding with the pod system for more support. At the end of the week, my average sleep score on the Oura Ring is 79 out of 100. According to Oura, that falls in the range of good sleep. I feel OK overall but don’t feel that refreshed when I jump out of bed. Some nights are restless, and I have trouble falling asleep when I get into bed.
But something strange has happened toward the end of this week. My body has started to wake up on its own within 30 minutes of my “scheduled” wakeup time. More than either of the two tools I tried, having a fairly consistent routine is starting to pay dividends.
Week 2: Trying out the sleep gadgets
Now that my sleep is in a more regular routine, it’s time to add on. I’ve heard a lot about the Therabody SmartGoggles that give heated massage around the temples, and on paper it sounds like a great experience. I’ll also use the “TikTok made me try it” $199 Hatch Restore 2, an alarm clock that simulates sunset and sunrise with colored light to help signal to your body when it’s time to sleep and when it’s time to wake up.

Wearing the SmartGoggles before bed.
I’m using the SmartGoggles in bed before I fall asleep. There’s a preset sleep mode at the touch of a button, or you can pair with the Therabody app for additional sleep routines. It takes me a few minutes to adjust to the sensation of a mechanical massage around my eyes, but once I feel the heat radiate onto my temples, I start to relax. At the end of the 15-minute session, you can see if your heart rate has lowered. Mine dropped from 82 to 66 beats per minute. You’re not supposed to sleep with the SmartGoggles on — they’re far too bulky. I slip them off feeling unusually calm and drift off to sleep.
Last week, the Oura Ring identified that my sleep latency wasn’t great — that’s the time between getting into bed and falling asleep. I think it’s because my mind is racing too much, so I’m also listening to meditations from the Centr app. I’ve chosen the Power Sleep sessions narrated by Chris Hemsworth. The SmartGoggles do make some mechanical noise so I need to listen with noise-canceling earbuds.
I keep coming back to one particular Power Sleep session called “Calm your worried mind.” The music that plays underneath Hemsworth’s voice is incredibly soothing. I can’t fall asleep with earbuds in, so after I’m done with the SmartGoggles, I put on the $143 Manta Sound Sleep Mask. It’s got adjustable blackout cups that do a great job of blocking out stray light in my bedroom, with thin built-in Bluetooth headphones so I can fall asleep listening to the meditation.
Sound plays an intriguing role in sleep, and different types of sound — often described as colors, such as white noise and brown noise — may reduce the time it takes for you to fall asleep.
“Our brain wave patterns slow down as we move from wakefulness to sleep,” says Hailey Meaklim, a sleep psychologist based in Melbourne, Australia, who helped develop Power Sleep. Sounds in the 0.8-2 Hz frequency, like those used in my favorite meditation, may enhance our sleep as they mimic brain waves during slow wave or Delta sleep, often referred to as deep sleep on your tracker. But she says the studies on this are limited and more research needs to be done.
The next evening, I walk into my bedroom just before 10 p.m. and see a gentle orange glow coming from the Hatch Restore 2. It’s a nice visual reminder to wind down and get ready for bed. Because my body is starting to wake up on its own, I don’t really use the sunrise light effect, but I can see how it would be helpful if you struggle to get out of bed in the morning with a traditional alarm.
The Restore 2 also offers guided audio sessions and nature sounds to aid relaxation, but I haven’t found them as effective as Power Sleep. Tonight, I’m listening to a session called The Endless Beach. I love hearing the sounds of the ocean alongside Thor’s dulcet tones, helping to release my mind from the worries of the day. Again, I drift off into a peaceful slumber.
Then reality strikes. My baby is starting to wake up again during the night, just like the newborn days. I spend a few hours intermittently through the night, walking back and forth between our rooms trying to get her to go back down. Sleep is a learned behavior, Pelayo tells me, so I’m helping her sleep even if it comes at a cost to me in the short term.
After this week, I tally up my sleep score and get an average of 81, in the realm of good sleep, according to Oura. It’s moving in the right direction, and I also feel slightly better, but I think that’s mostly because I’ve reduced my sleep latency and feel less stressed before falling asleep. And just as Pelayo tells me, even if I have an occasional night or two of bad sleep, it’s not the end of the world, and it doesn’t derail my progress.
Week 3: You can put a price on good sleep, and it’s $2,500
A giant 138-pound box covered in blue shrink wrap has just shown up at my door. Inside is The Curve, a $2,500 infrared sauna from Clearlight. There are three main components: an infrared amethyst mat with actual stones woven throughout and two vinyl domes that slide on top of you as you lie down. Each piece is individually temperature controlled. Unlike hot rock saunas, the dome’s infrared panels don’t produce steam. It’s a different kind of heat, more like the gentle sensation from a warm shower than the thick heat in a traditional sauna.

Taking a normal sauna is relaxing, but when you lie down it’s even better.
There is some evidence that sauna use may improve sleep. “The important thing is that it isn’t just to be looked at as a one-time shot,” says Raleigh Duncan, CEO of Clearlight. He adds that the sweet spot to take a sauna is around four times per week. He tells me that I should ease into it and start with short sessions because I’m trying to make a new habit. “And as we know, habits don’t like being forced.”
The idea is to take a sauna at night, ideally around 20 minutes, then have a cooldown period. Sit, relax, maybe take a shower if you sweat. This is when your body temperature will drop and melatonin — otherwise known as the sleep hormone — gets produced. Your body regularly produces melatonin on its own; here, the sauna is just helping it along.
In week three, I’m also trying another high-tech tool that touts temperature as the key to good sleep. The Eight Sleep Pod 3 is a water-based heating and cooling system that retrofits to any mattress, like a high-tech fitted sheet. It learns your sleep patterns to automatically adjust the temperature through the night. The idea is you’ll get better sleep because your temperature is regulated.
To get this week’s nightly routine started, I head to the garage to take my first infrared sauna. It’s bone-chillingly cold in San Francisco tonight, and as the sauna preheats, I shiver. Climbing into The Curve feels like entering a warm cocoon, and I’m soon feeling more relaxed than I have in a very long time. I don’t take a sauna every night, per Duncan’s recommendation, but I do use the Eight Sleep consistently. It takes two nights to tweak the temperature on the Pod 3 to my liking and I generally run cold, so having the bed at a warm +3 when I jump in, equivalent to a toasty 90 degrees Fahrenheit, is a nice treat.

The Eight Sleep on my bed.
I get some of my highest sleep scores yet, especially on the three nights this week when I take a sauna: My personal best is 93, and I feel strangely proud when I check the Oura app in the morning. But I still have some restlessness, so my average sleep score for the week is 83. I’m excited about nudging the numbers in the right direction, but more importantly I’m feeling more refreshed when I wake up and more energetic during the day.
Could part of this be down to a placebo effect? I ask Pelayo after I’ve had what I feel is a pretty solid week of sleep with my new gadgets.
“If you trust it, it will have a very strong placebo effect,” he says. “We noticed from sleeping pill studies, there’s about a 30% response just from getting the placebo. Because if you trust it, it’ll work because it lowers anxiety.”
Another promising trend I noticed this week: My heart rate variability is going up. That’s the time between heartbeats. HRV can be a good indicator of how much stress your body is under. There’s no one optimal value that applies to everyone, but mine is increasing slowly but surely. A higher value can indicate you’re getting good-quality sleep and your body has recovered from the day’s stresses.

A relaxing session in The Curve infrared sauna.
Sleep is the key to recovery
Sleep is the foundation of performing at your peak, whether you’re a fitness enthusiast or an Olympic-level athlete.
Lucy Schott is a CrossFit athlete and coach. She trains for at least an hour and a half every day and does 200 minutes of cardio-based exercise a week, but she noticed that poor sleep was seriously affecting her performance. “Pushing yourself to 80% of your maximum heart rate is quite difficult when you don’t have the energy or the capacity,” she says. “And so that’s when I started to investigate my sleep journey a little bit.”
Tracking with wearables like a Garmin watch and the Whoop band, she tried to boost her sleep quality by improving her sleep hygiene, putting her phone away before bedtime, taking melatonin supplements and looking at her nutrition. Her sleep improved only a little, so she sought out an at-home sleep test. It showed she got very little REM sleep and spent most of the night in light sleep. Using white noise or listening to a podcast sometimes helps. Like me, she’s experimented with different tools and techniques and is still on the hunt for a solution.
“I still wake up really tired, basically every day,” Schott says. “I’ve gotten used to it. But actually training helps a lot … It gives you energy somehow.”
Sleep tracking is great, unless it makes you feel worse
Almost every smartwatch and fitness tracker can track sleep when you go to bed. For me, it’s second nature to grab my phone in the morning and check how the night went. Some devices like the Oura Ring and Google Pixel Watch will give you a sleep score that ranks your rest. Samsung’s Galaxy Watch has sleep coaching, with tips on how to improve your sleep over several weeks. It also has snore detection when you go to bed with a Galaxy phone on your bedside table.
The Apple Watch is more about establishing and maintaining a sleep routine, rather than focusing on a particular sleep score, though it still tracks sleep stages, time in bed and other metrics like wrist temperature. It encourages you to set a sleep schedule and wind-down period, automatically activating a Sleep Focus mode that silences notifications and turns off the Apple Watch screen at night.
Wearables generally use an accelerometer to detect movement, maybe factoring in heart rate to calculate when we move between sleep stages. Some can take blood oxygen readings too. But there’s no universal methodology for tracking sleep on a consumer device, and they all calculate their sleep scores and sleep stages differently. I’ve worn multiple watches and rings to bed to compare results and been taken aback at how different they were when I checked results in the morning. Admittedly, at times I’ve become anxious because a tracker has told me I should be getting better rest, and I try to fix it for the next night. Or sometimes, the opposite happens where I get a “great” sleep score according to the tracker, but I feel like I’ve had a terrible night’s sleep.

One of my best sleep scores ever from the Oura Ring.
There’s a name for this phenomenon: orthosomnia. You get preoccupied about getting the right or correct sleep, obsessing over your data and trying to improve it.
Kelly Glazer Baron, a professor in the department of family and preventive measurement at the University of Utah, identified this phenomenon in 2017. “It was leading people to do things that were not great for their sleep,” she says. “So they were spending more time in bed trying to catch a little bit more sleep and squeeze more sleep out of their night. But when you have insomnia and you do that, your sleep becomes even more broken.”
Pelayo says more and more patients want to show him their sleep data. He tells me this has always been an issue, only the technology changed. People used to show up with 8-hour VHS tapes from night vision cameras, expecting him to sit and watch their sleep.
The real value comes when you use trackers over time to identify trends, rather than obsess over particular numbers each night. They’re a tool and not the be all and end all of determining if you got quality sleep. After all, they can’t tell us how we feel. Yet.
“I also tell my patients that how you feel during the day isn’t just about what happened at night,” says Baron, so tracking time in bed isn’t the only thing to keep an eye on. It’s also important to look at mental and physical strain, as well as stress. But, she says, “they’re not exactly measurable, at least [not] how we’re doing things right now.”
Deep sleep is something that all our sleep trackers tell us is important. I’m used to waking up and seeing some pretty dismal numbers: 30 minutes here, 43 minutes there. But slow wave sleep only accounts for about 10% of the total night’s rest according to Pelayo, while REM sleep is about 20% to 25% of the night.
“People often ask what’s the most important part of sleep: Is it the light sleep, intermediate sleep, deep sleep or REM sleep?” he says. “And it’s like asking which part of your transmission matters the most: the whole thing matters.”
Another important factor to remember is that wearables can’t detect clinical sleep disorders. But the Galaxy Watch is getting FDA-approved sleep apnea detection later this year, and it’s rumored the next Apple Watch may do the same.
Subscriptions are everywhere, even for sleep
Sleep tracking is becoming a lucrative add-on for many consumer tech companies. For example, both Fitbit and Oura lock most of their useful sleep data behind paid monthly subscriptions: $10 a month for Fitbit Premium and $6 a month for Oura (both offer free trials for a limited period). Fitbit shows your sleep score and sleep stages without a Premium subscription, but if you want personalized sleep insights, a sleep score breakdown, a monthly sleep profile and a wellness report you’ll need to pay. The Oura ring is even more limited without a subscription: you get only a sleep, readiness and activity score.
Whoop, a fitness and health wearable designed for athletes, has a different model. Its $20 monthly subscription subsidizes the cost of the device, but if you cancel the subscription you have to send it back. The Hatch Restore 2 and Eight Sleep also require subscriptions to unlock most of their key features. You may be able to put a price on good sleep, but then you’ll need to keep paying for it.
My sleep test results
I’ve been tracking my sleep for years with a range of smartwatches, fitness trackers and smart rings. They’ve all said it falls within a normal range. Over the three weeks of my personal sleep experiment, I see steady progress on the Oura Ring, with a string of blue lines against almost all metrics (blue is good, red is not so good). But I don’t feel dramatically refreshed despite improving my sleep habits. So I’ve put it down to the exhaustion that comes with becoming a mom and don’t expect any anomalies on my sleep test. After all, my tracker says I’m doing fine. Maybe this feeling is all in my head.
Back in the sleep lab, Jonathan pops his head in at 7:30 a.m. to wake me up. Off come all the electrodes, bands and sensors. I shower to wash off the adhesive before Pelayo shows me last night’s results. “You have really pretty sleep architecture,” he says as I feel strangely proud of the graph he lays out in front of me. He shows me how all my sleep stages fall in normal ranges: I get a touch more REM sleep, and deep sleep makes up 9% of my night.
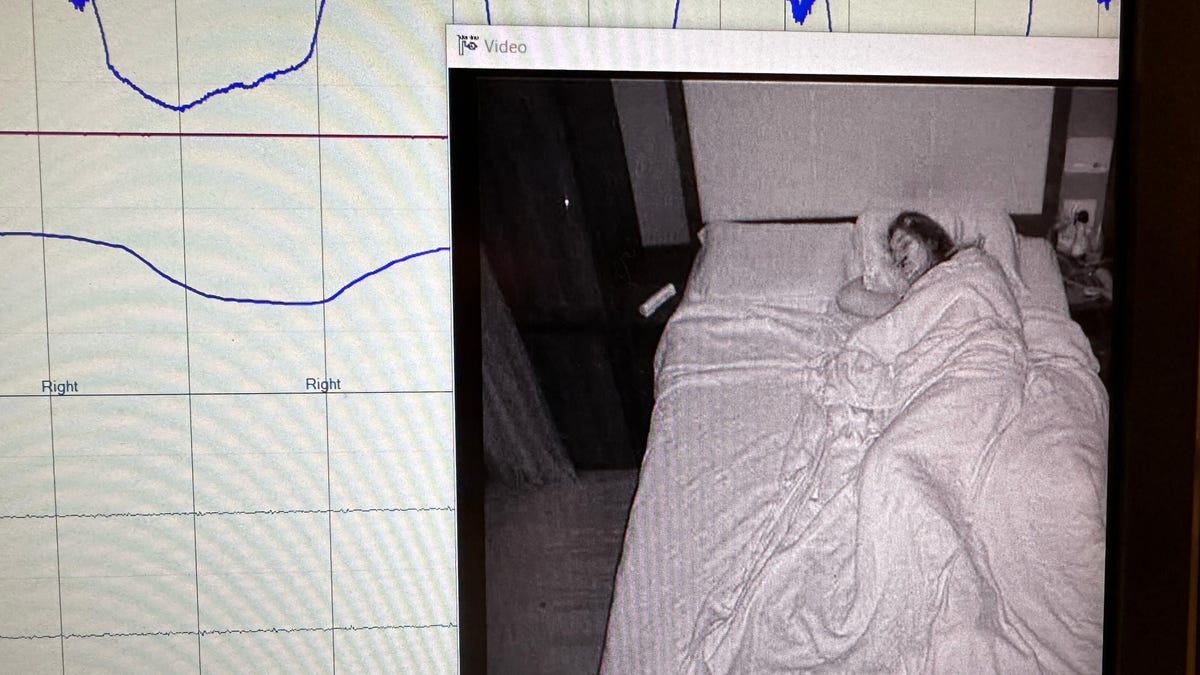
When a doctor or sleep technician reviews your rest, they can see footage of your sleeping and data like brainwaves, breathing and heart rate during your sleep stages.
Then he explains the main abnormal finding. My legs kicked 136 times during the night, interrupting my sleep. I look further down the sheet of paper in shock and see a string of metrics highlighted in red. “People with periodic limb movements are often not aware that something is wrong with their sleep,” he says.
Pelayo can’t diagnose my sleep condition, given I did a sleep test for the purposes of this story and wasn’t an actual patient. But all signs point to restless leg syndrome, a neurological condition that makes you feel like you need to move your legs. It’s one of the 80-plus sleep disorders and likely explains my sleep woes, even if it is mild. After I leave the center, I make an appointment with my primary care physician to see if there’s something I can do or if it’s something I just need to be aware of.
As much as I wanted to get a perfect sleep score during this experiment, I can see now why that was nearly impossible. None of the tech I tried could have caught (or alleviated) this phenomenon.
How to get better sleep
We all need sleep, but how we sleep is highly personal. What works for me might not be the right solution for you, so I asked all the sleep experts I spoke with for some general recommendations.
Pelayo says people who experience insomnia often try to do very logical things like staying in bed to rest if they can’t sleep. But resting and sleeping are two different things. If your body needs only 7 hours of sleep, yet you spend 10 hours in bed, the result is very light sleep. It seems counterintuitive, but in this case one way to get deeper sleep could be by spending less time in bed.
“Initially, what will happen is that you’ll still wake up in the beginning, but eventually your body’s going to sleep deeper,” he says. “It’s like lifting weights in a sense, you’re gonna stress that ability.” Plus, you’re not wasting 3 hours every night.
It sounds obvious, but making yourself as comfortable as possible can also help. While I loved having the Eight Sleep adjust my bed temperature automatically, it’s a sleep investment that might be out of reach for many.
“We don’t prescribe a pillow,” Baron tells me, but she explains that small, inexpensive tweaks to your sleep environment like breathable pajamas, bedding and even earplugs can make all the difference depending on your sleep issues.
Meaklim says it’s really helpful to reduce the worry and anxiety around sleep through meditation or other relaxing habits. That can promote trust in our body and mind that we can get the sleep we need. “We don’t have to do too much to try and control it,” she says.
Please remember if you’re experiencing any sleep issues, it’s important to talk to your medical provider.

The Somnox 2 sleep robot (left), Aura Circle smart sleep mask (center) and Manta Sleep Sound Mask (right).
Learning how to sleep better takes time. I could dedicate only three weeks to my experiment for the purposes of this story, but I’m going to keep up my new sleep habits because I saw real progress and it’s an investment in my overall health. Setting a clear wakeup time was the most helpful foundation because I could work backward and set my bedtime accordingly. If things didn’t go to plan (and they didn’t, thanks to my baby’s sleep regression), I could always take a nap or shift my timings on weekends to sleep a bit later. Naps are a bit like snacking, Pelayo tells me: As long as it doesn’t spoil your dinner, it can be a good thing.
“A short nap should be refreshing to make you feel better,” he says, and the key is to keep naps between 20 and 40 minutes at most.
I tried a lot of sleep gadgets during this process. Some made a clear difference in how I felt. I’d been skeptical about how effective the Therabody SmartGoggles would be, but they really helped me relax and signaled to my body that it was time to unwind. The Eight Sleep Pod 3 was great for regulating my temperature, as I often wake up too cold or too hot. Having it adjust automatically during the night definitely kept me asleep for longer. The Clearlight sauna was the weirdest, yet most rewarding, sleep tool I tried because I could feel my entire body relaxing and easing into sleep after each use. Some nights, I almost fell asleep in the sauna because I was in such a blissful state.
But it’s the least expensive tool that will stick with me long after I put this whole experiment to bed: sound. The Power Sleep meditations were particularly effective in putting me in a relaxed state thanks to the combination of music and voice. Even if you don’t want to spend money on a dedicated app, listening to relaxing music or any number of YouTube meditations could also be beneficial.
We all sleep differently, so what works for me may not work for you. But if it doesn’t break the bank, it’s definitely worth exploring. After all, a good night’s sleep is priceless.
Senior Motion Designer | Amy Kim
Video | Lexy Savvides, Chris Pavey, Andy Altman, John Kim
Senior Project Manager | Danielle Ramirez
Director of Content | Jonathan Skillings


