This work may not be copied, distributed, displayed, published, reproduced, transmitted, modified, posted, sold, licensed, or used for commercial purposes. By downloading this file, you are agreeing to the publisher’s Terms & Conditions.
ABSTRACT
Medical and neuropsychiatric benefits associated with physical exercise and activity are well recognized. It is less well known that time spent in sedentary behaviors, such as television-viewing or sitting at a desk, are associated with adverse health outcomes even after taking into consideration health-related physical activity. Although sedentary behaviors have become common in daily life, people tend to substantially underestimate how sedentary they actually are. The average person spends nearly 10 hours per day in a sedentary state, during leisure activities or work; sedentariness is even greater in persons with major mental illness such as psychosis. This article explains what sedentariness is, why sedentary behaviors are common in daily life, and how sedentariness is defined and assessed. Sedentariness is an important concept in its own right; it is not merely an absence of health-related physical activity. Sedentariness is associated with adverse outcomes in children and adolescents, adults, and older adults. Examples are provided of associations between sedentariness and adverse medical outcomes such as the metabolic syndrome, cardiovascular disease, stroke, and all cause mortality. Examples are also provided of associations between sedentariness and adverse mental health outcomes such as anxiety, depression, and dementia. Importantly, the adverse associations are independent of health-related physical activity; however, higher levels of physical activity may attenuate or offset the adverse effects of sedentariness. It is hoped that this article will encourage readers to reduce sedentary behaviors with a view to improve long-term physical and mental health.
J Clin Psychiatry 2024;85(1):24f15261
Author affiliations are listed at the end of this article.
The World Health Organization 2020 guidelines on physical activity and sedentary behavior1 discourage sedentariness and recommend at least 150–300 minutes of moderate intensity aerobic exercise per week, or at least 75–150 minutes of vigorous aerobic exercise per week, or equivalent combinations thereof, for the promotion and maintenance of health. If we ambitiously take the highest number, 300 minutes per week, it averages to nearly 45 minutes of exercise per day; that still leaves us with about 23 hours remaining in the day. If we remove a further 9–10 hours for sleeping, eating, and other basic daily activities, we’re left with 13–14 waking hours.
In present day life, most of these 13–14 hours are spent in sitting or other sedentary behavior. As examples, many people work at a desk and so sit for perhaps 6–8 hours per day. Many people commute to work, seated in private or public transport, for 1–2 hours per day. Many children and adults use smartphones, watch television, play video games, or merely read, seated, for several hours a day; so, even leisure and pleasure recreational activity is sedentary. At best, these 13–14 hours may include fidgeting, or short periods of walking inside a house or the workplace, or walking to and from transport points.
Studies confirm that, among adults, including older adults, sedentary behavior occupies much of waking life. For example, in a nationwide survey2 of 2,640 US adults (mean age, 45 years; 51% female), mean sedentary time was 9.5 h/d, as assessed using a validated, self-administered, previous-day recall questionnaire. Most of the sedentary time was accumulated during leisure (47%) and work (16%). In a large study3 of 49,841 older adults (mean age, 67 years; 55% female) in the UK Biobank, the findings were almost identical: the median sedentary time was 9.3 h/d. Readers may note that these data indicate that half of the sample in each study was sedentary for approximately 9.5 h/d or longer; in persons with psychosis, higher levels of sedentariness, up to an average of 12 h/d, are reported.4
Given the importance of physical activity for health, explained in earlier articles in this series,5,6 it would seem that excessive sitting and sedentary time, as the opposite of physical activity, could be detrimental to health. This has indeed been suggested. The present article therefore explains what sedentariness is, what behaviors do and do not comprise sedentariness, and how sedentariness is assessed. Examples are provided of associations between sedentariness and adverse physical and mental health outcomes. The purpose of this article is to encourage reductions in sedentary behaviors and not to comprehensively review the literature in the field.
What Sedentariness Is
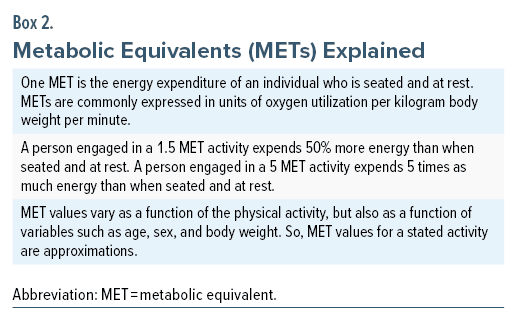
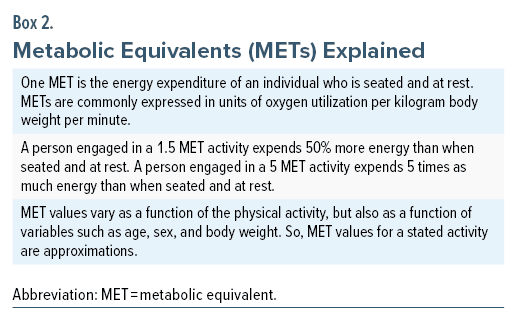
It may seem that sedentariness is merely the absence of physical activity and so does not need to be independently researched; that is, measuring and studying sedentariness is merely measuring and studying physical activity in a different way. This is not true because there are distinct definitions for what constitutes sedentariness and for what constitutes physical activity that contributes to health. This is explained in Box 1; the concept of metabolic equivalents, explained in Box 2, is invoked. Metabolic equivalent values for a wide range of activities have been published.7
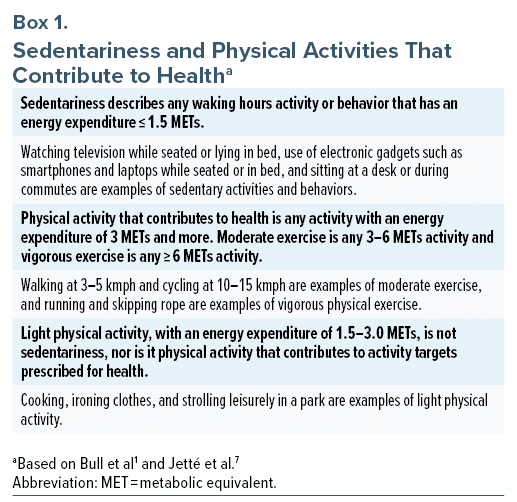
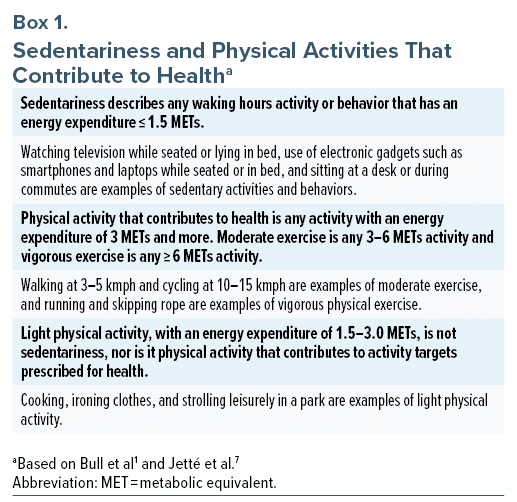
It is important to observe that a lifestyle replete with light physical activity, such as puttering around in the house or garden, or frequently moving around at the place of work, may not meet physical activity targets prescribed for health; however, such a lifestyle is not sedentary, either. The distinction is important because sedentariness, independent of levels of health-related physical activity, has been associated with adverse health outcomes in observational studies. This is why sedentariness and physical activity need to be independently researched in health-related contexts.
Assessment of Sedentariness
Sedentariness is best assessed by actimetry, using standardized electronic devices. This is because people often underestimate how sedentary their lifestyle is. For example, in a systematic review and meta-analysis of 123 studies (pooled N = 55,199), Prince et al8 found that, on average, relative to device measures, people underestimated their sedentariness by 105 min/d. This is easily explained; detailed daily logs of physical activity are necessary to accurately capture the extent of sedentariness, and people do not keep such logs. So, their guesstimates are inaccurate. This means that there is no room for complacency; people may be more sedentary than they realize they are.
It may be noted that commercial devices that measure activity may not be accurate; different manufacturers use different algorithms that were differently validated; and there may be inaccuracies related to where on the body the device is worn, how well-fitting it is, whether body sweat interferes with signal detection, and other matters. In contrast, actimeters or accelerometers used in research are usually standardized before use.
Sedentariness and Physical Health
Sedentary time is a risk factor for the metabolic syndrome (MetS), a condition that lies along the path to many health disorders. In a systematic review and meta-analysis of 4 prospective cohort studies and 22 cross-sectional studies (N = 105,239), Wu et al9 found that total sedentary time was associated with an increased risk of MetS at both intermediate (median, 4.1 h/d; odds ratio [OR], 1.17; 95% confidence interval [CI], 1.08–1.26) and high (median, 7.3 h/d; OR, 1.71; 95% CI, 1.43–2.04) levels. Total screen time was also associated with an increased risk of MetS at both intermediate (median, 2.2 h/d; OR,1.20; 95% CI, 1.10–1.32) and high (median, 3.4 h/d; OR, 1.63, 95% CI, 1.44–1.86) levels. The association between sedentariness and MetS was stronger in women.
Sedentariness has been associated with an increased risk of medical conditions and premature mortality. For example, in a systematic review and meta-analysis of sedentary time and the risk of cardiovascular disease, Pandey et al10 identified 9 prospective cohort studies (pooled N = 720,425) with a median follow-up of 11 years. Subjects in the highest sedentary time category (median, 12.5 h/d) were at increased risk of incident cardiovascular disease events (hazard ratio [HR], 1.14; 95% CI, 1.09–1.19) relative to subjects in the lowest sedentary time category (median, 2.5 h/d). Increased risk was observed only at higher (sedentary time > 10 h/d) levels of sedentariness. In another systematic review and meta-analysis of 7 prospective cohort studies (pooled N = 677,614) with a median follow-up of 12.2 years, Wang et al11 found that sedentariness was associated with an increased risk of stroke only from a threshold sedentary time of 11 h/d (HR, 1.21; 95% CI, 1.12–1.31).
Ekelund et al12 described a methodologically important systematic review and meta-analysis of 8 prospective cohort studies (pooled N = 36,383) with a median follow-up of 5.8 years. This study was unique because the authors of each of the contributing studies were asked to harmonize their accelerometry-based information and to redo their analyses in accordance with uniform definitions and methods provided to them by the meta-analysis authors. There was a clear dose-response effect. Relative to the least sedentary quartile, the all cause mortality risk increased, quartile by quartile, to HR = 1.28 (95% CI, 1.09–1.51), HR = 1.71 (95% CI, 1.36–2.15), and HR = 2.63 (95% CI, 1.94–3.56). Relative to a sedentary time of 7.5 h/d, increased all cause mortality reached statistical significance at a threshold of about 9.5 h/d. The HRs were 1.48 (95% CI, 1.22–1.79) at a sedentary time of 10 h/d and 2.92 (95% CI, 2.24–3.83) at 12 h/d. These results remained similar in analyses that addressed reverse causation, in which deaths during the first 2 years of follow-up were excluded.
Sedentariness and Mental Health
Sedentariness has been associated with an increased risk of psychiatric disorders in children as well as in adults. For example, in a systematic review and meta-analysis of 13 observational studies (pooled N = 70,425) conducted in pediatric (5 studies) and adult (8 studies) subjects, in both unadjusted (OR, 1.33; 95% CI, 1.14–1.55; 7 studies) and adjusted (OR, 1.48; 95% CI, 1.25–1.75; 7 studies) analyses sedentariness was found to be associated with anxiety symptoms or anxiety disorder.13
In another systematic review and meta-analysis of 16 observational studies (pooled N = 221,599) subjects, the highest vs lowest category of sedentary behavior (relative risk [RR], 1.42; 95% CI, 1.22–1.67; 9 studies) and the highest vs lowest category of television-watching time (RR, 1.26; 95% CI, 1.14–1.40; 5 studies) were both associated with a higher risk of depression. In both analyses, the risks were dose-dependent.14
In a systematic review and meta-analysis of 58 longitudinal studies conducted specifically in children and adolescents, sedentary behavior and television-watching were associated with an increased risk of anxiety (OR, 1.23; 95% CI, 1.11–1.35) as well as depression (OR, 1.14; 95% CI, 1.08–1.20).15
In these meta-analyses, although the pooled risks are small, they are clinically significant because anxiety and depression are common in the population; so, even a small increase in risk translates into a meaningful increase in population prevalences.
Sedentary behavior has also been associated with an increased risk of incident dementia among older adults3; this study has many points of interest and will be the subject of discussion in the next article in this column.
Offsetting Sedentariness Risks Through Physical Activity
Some sedentariness is inevitable in daily life. Most people sit when they eat, commute, and work for their living. Most people sit when engaged in necessary phone-related activity. Many people unwind seated, by engaging in screen time with their smartphones or television sets. As reviewed in earlier sections, such sedentariness is associated with adverse physical and mental health outcomes regardless of health-related physical activity. However, can increased physical activity offset the harms of sedentariness? If yes, this would be of comfort to those who cannot avoid sedentariness in their daily life.
In this regard, in a meta-analysis of 9 prospective cohort studies (pooled N = 44,370), Ekelund et al16 harmonized accelerometry assessments and data analyses. They found that, in subjects with low levels of physical activity, low (HR, 1.65; 95% CI, 1.25–2.19), medium (HR, 1.65; 95% CI, 1.24–2.21), and high (HR, 2.63; 95% CI, 1.93–3.57) sedentariness were associated with a significantly increased risk of all cause mortality. Importantly, they also found that, in subjects with high levels of physical activity, neither medium (HR, 1.16; 95% CI, 0.87–1.54) nor high (HR, 1.40; 95% CI, 0.87–2.26) sedentariness was associated with a significantly increased risk of all cause mortality.
In these analyses, the reference group comprised the ideal: subjects with the lowest level of sedentariness combined with the highest level of moderate to vigorous physical activity. The median sedentary time (min/d) was 8.5, 9.5, and 10.7 h/d across tertiles, and the median moderate to vigorous physical activity time was 2.3, 11.2, and 34.3 min/d across tertiles.
Physical activity may offset adverse health outcome associations with sedentary time in pediatric populations, as well. For example, in a systematic review and meta-analysis of 8 studies of the International Children’s Accelerometry Database (pooled N = 6,009), Renninger et al17 found that a per-day 10-minute increase in moderate to vigorous physical activity (OR, 0.88; 95% CI, 0.82–0.94) and vigorous physical activity (OR, 0.80; 95% CI, 0.70–0.92) were each associated with lower risk of the MetS; in contrast, a 1-hour increase in sedentary time was associated with an increased risk of the MetS (OR, 1.29; 95% CI, 1.13–1.45). Importantly, the benefits associated with moderate to vigorous physical activity persisted after adjustment for sedentary time (OR, 0.91; 95% CI, 0.84–0.99); and the harms associated with sedentary time were attenuated after adjustment for moderate to vigorous physical activity (OR, 1.14; 95% CI, 0.96–1.36).
Take-Home Message
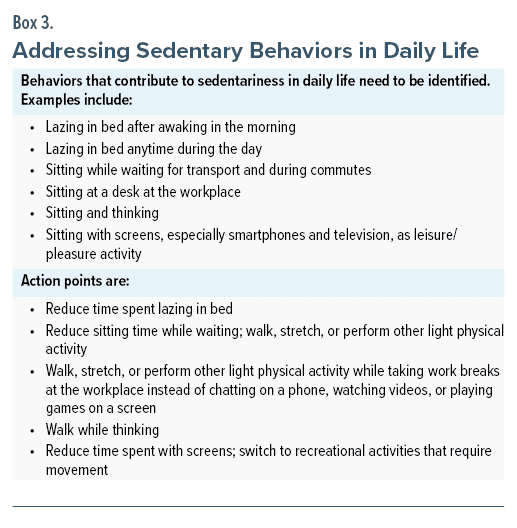
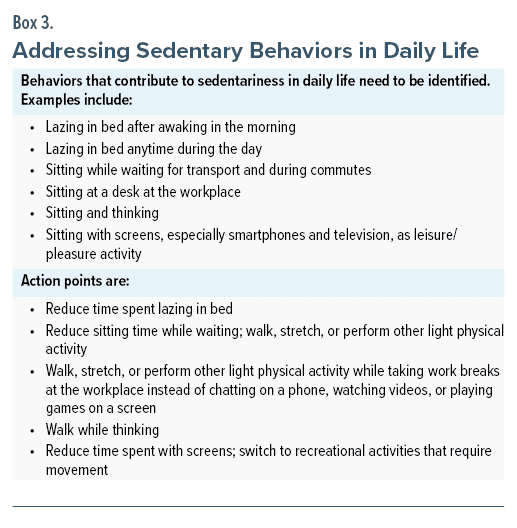
Increased sedentary time is associated with poorer physical and mental health outcomes even in people who exercise regularly. Although this conclusion is based on the findings of observational studies, it would be prudent to reduce sedentary behaviors (Box 3). Some sedentariness is unavoidable, such as sedentariness associated with commuting or working at a desk. However, it is possible to attenuate the possible adverse health outcomes of sedentariness by increased engagement in physical activity.
Parting Notes
Many studies have demonstrated adverse health outcomes associated with sitting time,18 screen-viewing time,19 and, more specifically, even television-viewing time.20 Sitting time is a subset of sedentariness; it would not include, for example, time spent in bed after awaking or time spent lying in bed and reading or viewing a screen device. Screen time is (largely) a subset of sitting time and television time is a subset of screen time.
Sitting time, screen time, and television time studies are important because they draw attention to specific problematic lifestyle activities. The sedentariness studies are important because they draw attention to overall lifestyle behavior.
Finally: the focus of this article is on sedentariness as inactivity, and so this article does not address potentially harmful changes in mental health that have been associated with different kinds of screen time and different screen time contents and activities. Such effects merit independent consideration.
Article Information
Published Online: January 29, 2024. https://doi.org/10.4088/JCP.24f15261
© 2024 Physicians Postgraduate Press, Inc.
To Cite: Andrade C. Physical exercise and health, 5: sedentary time, independent of health-related physical activity, as a risk factor for adverse physical health and mental health outcomes. J Clin Psychiatry. 2024;85(1):24f15261.
Author Affiliations: Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India (candrade@psychiatrist.com).

 Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.
Each month in his online column, Dr Andrade considers theoretical and practical ideas in clinical psychopharmacology with a view to update the knowledge and skills of medical practitioners who treat patients with psychiatric conditions.Department of Clinical Psychopharmacology and Neurotoxicology, National Institute of Mental Health and Neurosciences, Bangalore, India (candrade@psychiatrist.com).
Financial disclosure and more about Dr Andrade.


