NEW YORK (AP) — Elisa Reyes has been coming to Plaza del Sol Family Health Center for doctor's appointments for more than a decade. She moved a while ago, but she still comes back even if it takes two hours round trip by bus.
That's because her two children see the same doctor. Because when she's sick, she can come in without an appointment. Because the staff at Queen's Clinic helped her apply for health insurance and food stamps.
“I feel like I'm at home. They also speak my language,” Reyes, 33, said in Spanish. “I feel comfortable.”
Plaza del Sol is one of 20 facilities operated by Urban Health Plan Inc., one of approximately 1,400 federally designated community health centers. One out of every 11 Americans relies on them for regular medical care, social services and, in some cases, fresh food.
Clinics serve as an important safety net for low-income people of all ages in every state and U.S. territory. But it's a safety net under stress.
Since 2012, community health centers have seen a 45% increase in the number of people seeking care, opening more and more service sites and expanding their footprint to more than 15,000 locations.
Many centers are understaffed and are struggling to find doctors, mental health professionals, nurses and dentists. Leaders also told The Associated Press that months of debate over the federal budget have made funding a constant concern, making long-term planning and hiring nearly impossible. .
Community health centers have existed in some form for decades and are largely what remains when urban and rural hospitals close or reduce services.
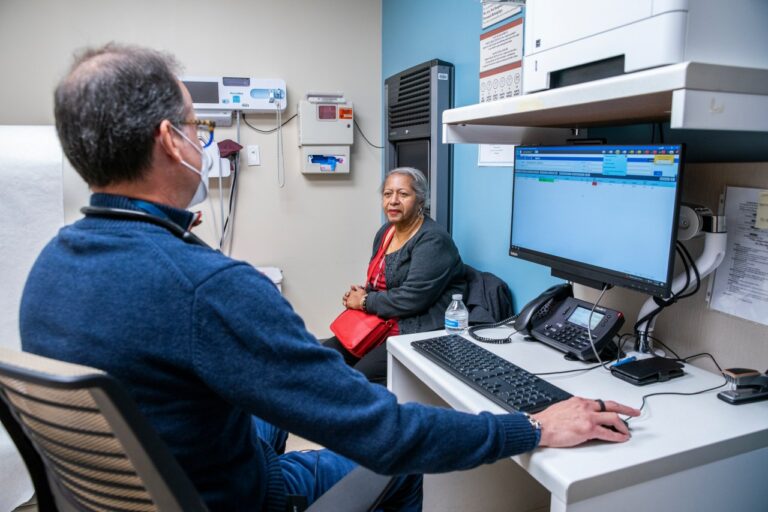
Dr. Matthew Kusher, Plaza del Sol's clinical director, said people live in apartments, one family per room, to stop the spread of influenza and COVID-19 when isolation is not possible. He said that there are some things that cannot be changed with a prescription.
“What we provide here is only 20 percent of what goes into someone's health,” Kusher said. “Their health is highly determined by other factors, including poverty and lack of access to food, clean water and healthy air.”
According to the U.S. Health Resources and Services Administration, nine out of 10 health center patients live at or below 200 percent of the federal poverty line. More than that:
— In 2022, approximately 1.4 million health center patients became homeless.
— One in five people had no insurance.
— Half received Medicaid.
— One in four people were best served in a language other than English. Approximately 63% were racial or ethnic minorities.
Dr. Aklema Mohamad began working as a medical assistant at Urban Health Plan's first clinic, San Juan Health Center, 50 years ago. She has taken care of several families over her three generations.
“I'm so blessed to work in this community. When I walk through the door or walk down the street, I get hugs,” she said. “I keep saying, 'Oh, Dr. Mo! You're still here!'”
Muhammad's biggest problem is staffing. After the worst of the pandemic, many pediatricians retired or took other jobs. It's not just about money. Job seekers tell her they want quality of life and flexibility.
“It's a tough job and a big problem because we have so many sick children and so many sick patients. But to take care of them… We don’t have enough health care providers,” Mohammad said.
Telemedicine can also be helpful, she said, with a former pediatrician sometimes offering virtual consultations to help alleviate symptoms. However, when telemedicine is not possible, El Nuevo San Juan Health Center strives to provide care to people instead.
About 150 seniors are receiving home visits, said Dr. Manuel Vasquez, vice president of medical affairs at Urban Health Plan, which oversees the program. Sometimes the care isn't covered, but the team does it for free.
“We said, 'No,' we need to do this,” he said.
Build community trust
In the wake of the Civil Rights Movement's Freedom Summer, the nation's first community health center opened in the Mississippi Delta in 1967.
Today, Delta Health Center in Mound Bayou, Mississippi, has 17 locations in five counties, including free-standing clinics and some within schools.
Temika Simmons, Delta Health Center's chief communications officer, said access to preventive care is important as area hospitals cut neonatal services and other specialty care.
“If you're in the middle of a heart attack, you might die on the way because you have to be airlifted to Jackson or Memphis, where they have the equipment to save your life,” she says. “So what we've done with primary care is try to move people away from the primary care field.”
Another key to the center's ability to improve health disparities is understanding and becoming part of the community. Plaza del Sol is located in New York City's Corona District, which has become the epicenter of the coronavirus outbreak, in a neighborhood with a large Latino immigrant population. Staff must speak Spanish.
Simmons said Mississippi Delta staff are trained to spot signs of abuse and know when patients are “hustling and fighting” to fill out forms they likely can't read.
Center leaders say they are putting in as much money as they can to continue serving the community in the way they want, but more is needed.
Given patient volume growth and inflation in the medical sector, federal funding for centers would need to increase by $2.1 billion to match 2015 funding levels, according to an analysis sponsored by the National Association of Community Health Centers. That's what it means.
“Don't let the problems overwhelm you,” Simmons says. “You just have to take it one day at a time, one patient at a time.”
___
Associated Press data journalist Kasturi Pananjadi contributed to this report.
___
The Associated Press Health and Science Department receives support from the Robert Wood Johnson Foundation. AP is solely responsible for all content.