- Severe mental health conditions present challenges to both patients and healthcare professionals with the metabolic side effects of antipsychotic drugs.
- A pilot study from Stanford Medicine suggests that combining a ketogenic diet with standard medications may improve both metabolic health and psychiatric symptoms in people with severe mental illness.
- Despite these encouraging findings, experts emphasize the need for more comprehensive research and recommend adhering to more sustainable dietary patterns.
Mental health affects estimates
Although antipsychotics are essential for symptom management, they often cause metabolic side effects such as weight gain and insulin resistance, which negatively impact an individual's quality of life and, in some cases, lead to treatment discontinuation.
To address these challenges, Stanford Medicine recently investigated through a pilot study whether a ketogenic diet can improve metabolic and psychiatric outcomes in patients with severe mental illness.
Ketogenic diets, which are high in fat, low in carbohydrates, and moderate in protein, have been shown to be effective in managing a variety of conditions, including:
Now, a preliminary study from Stanford Medicine shows that using standard medications and treatments, a four-month ketogenic diet intervention significantly improves symptoms and quality of life in people with severe mental illness and metabolic disorders. It was found that there is a possibility that
This study psychiatric research.
This four-month study included adults diagnosed with bipolar disorder (76%) or schizophrenia (24%), taking antipsychotic medications, and who are overweight or have metabolic problems such as insulin resistance. 21 people participated.
Most participants were female (62%) and Caucasian (76%), with an average age of 43 years.
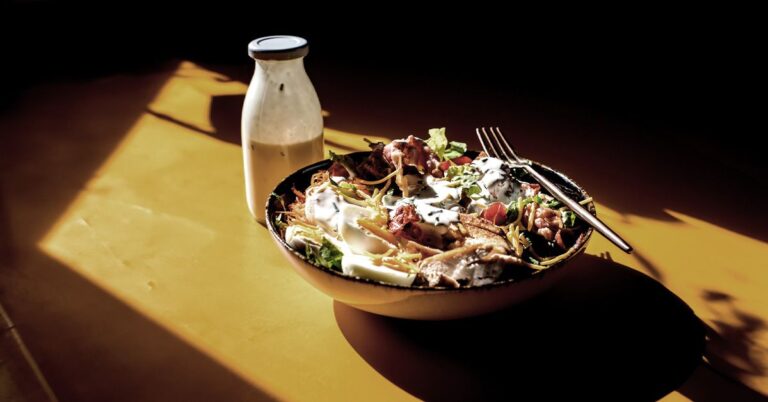
As outpatients, participants were instructed to follow a ketogenic diet with specific macronutrient ratios: 10% carbohydrates, 30% protein, and 60% fat.
Although they weren't required to count calories, they were asked to eat a minimum of 1,200 calories each day and limit their net carbs to about 20 grams a day.
Participants received a one-hour training session, educational materials, a ketogenic cookbook, recipes, and a personal coach to help with dietary adherence.
Dietary guidance included recommended daily intakes of vegetables, salads, and water, as well as instructions on measuring blood ketone levels.
The researchers checked dietary compliance weekly using a blood ketone meter. The study included regular medical and psychiatric evaluations by a psychiatrist, with additional confirmation from the participant's personal psychiatrist when possible.
Participants maintained their usual psychiatric care and medications for the duration of the study.
Of the 21 participants, 14 followed a strict ketogenic diet. These people had fewer cases of schizophrenia, had a shorter duration of illness, and had less severe psychotic symptoms than the semi-adherent group.
The semi-adherent group had higher rates of obesity, worse cholesterol levels and longer duration of illness.
Today's medical news We spoke with nutritional psychiatrist and author Uma Naidu, MD, who was not involved in the study and said, “The details of the ketogenic diet can be a challenge for some individuals.'' ” shared the opinion.[s] These more serious diseases need to be managed. ”
This may explain why people with more severe symptoms have lower dietary adherence.
Initially, 29% of participants met criteria for metabolic syndrome, and more than 85% had multiple medical conditions, including obesity, hyperlipidemia, and prediabetes. By the end of the study, no participants met criteria for metabolic syndrome, suggesting that the ketogenic diet had a positive impact on metabolic health.
On average, participants reduced weight and BMI by 10%, waist circumference by 11%, body fat mass index by 17%, systolic blood pressure by 6%, and improved metabolic markers such as visceral fat and inflammation. , HbA1c, triglycerides, and insulin resistance.
High levels of ketone bodies suggest greater dietary compliance and correlate with better metabolic health.
Psychiatric improvements were also significant, with a 31% reduction in the severity of mental illness.
Additionally, 79% of participants who had symptoms at the start showed significant improvement in their mental status, especially those who adhered to the diet.
Life satisfaction, overall functioning, and sleep quality were also reported to be improved, highlighting the wide range of positive effects of diet.
Research results suggest that a ketogenic diet may reduce psychiatric symptoms and reduce the metabolic side effects of antipsychotic drugs.
However, Naidoo advised caution when interpreting the results due to the small size of the study and the lack of a control group.
MNT We also spoke with Dr. Jasmine Thorne, a board-certified psychiatrist who was not involved in the study, to learn more about the ketogenic diet's potential to improve mental health through changes in brain chemistry and energy metabolism.
By shifting the brain's energy source from glucose to ketone bodies, the diet “may improve mental health outcomes such as mood stabilization and cognitive function,” she explained.
Research shows that this metabolic change may also improve psychiatric symptoms due to decreased metabolism.
Eliza Whitaker, MD, RD, a registered dietitian who was not involved in the study, emphasized the benefits of the ketogenic diet.
He noted that improving blood sugar and insulin sensitivity may also reduce psychiatric symptoms associated with metabolic problems.
Additionally, ketosis may improve symptoms
However, Professor Whittaker cautioned that more research was needed to fully understand the impact of a ketogenic diet on mental health, and also noted that symptoms could return if the diet was stopped.
Although antipsychotic drugs are effective in managing psychiatric symptoms, they often have side effects such as weight gain, diabetes, and increased risk of metabolic syndrome, posing a health dilemma for patients.
In this research, “[t]The significant improvements observed in both psychiatric and metabolic outcomes suggest that: [the ketogenic diet] “This could be a viable and effective adjunctive treatment in conjunction with psychiatric medications,” Thorne said.
However, she explained:
“The ketogenic diet is not commonly recommended as an adjunct therapy for the treatment of schizophrenia or bipolar disorder due to limited research, but preliminary research suggests it may have potential benefits.” It has been suggested that, like other areas of the medical field, this is a developing issue and is worth considering further afield. ”
Naidoo agrees, saying that for some people with bipolar disorder or schizophrenia, a ketogenic diet can be helpful, but it can mean stopping medications or changing treatment without a doctor's guidance. I made it clear that it wasn't.
Health care professionals should carefully monitor and adjust the combination of dietary approaches to psychiatric treatment to ensure safety and effectiveness.
Despite early positive results, the long-term sustainability of the ketogenic diet remains a significant concern among researchers and medical professionals.
Mr Thorne warned:
“Long-term use of a ketogenic diet to manage mental illness can lead to potential nutrient deficiencies and changes in the gut microbiome. Research is limited.”
Sanam Hafeez, M.D., a New York City neuropsychologist and director of Comprehend the Mind, who was not involved in the study, also said that the ketogenic diet expressed concern about the potential long-term effects of Development of eating disorders due to dietary restrictions.
Hafeez recommends considering sustainable, long-term dietary approaches such as Mediterranean diets and plant-based diets, as well as mindful eating and personalized nutrition for broader health benefits. Did.
Thorne also advised people to follow “science-backed recommendations for improving mental health through diet.”[ing] Focuses on a balanced diet rich in fruits, vegetables, lean protein, healthy fats, and whole grains while minimizing intake of processed foods, sugar, and excess caffeine . ”
“Incorporating foods rich in omega-3 fatty acids, magnesium, and probiotics may also support mental health,” she added.
Whittaker agreed, suggesting that “incorporating fermented foods such as kimchi, sauerkraut, and yogurt may improve mental health.”
It's important to eat a diet rich in whole foods and check with your doctor to make sure you don't have any nutrient deficiencies that could affect your health.
This pilot study on the effects of a ketogenic diet on schizophrenia and bipolar disorder shows promise for dual metabolic health and management of psychiatric symptoms.
Still, Dr. Thorne said larger randomized controlled trials are needed to validate these initial findings and understand the long-term effects of the ketogenic diet in psychiatric treatment.
Additionally, because the study lacked participants' dietary histories, Whittaker noted that any improvement could be due to participants improving their overall diet quality during the observation period.
This highlights the importance of understanding the context surrounding dietary interventions in mental health.
Despite the study's limitations, Whittaker concluded:[o]Overall, it's exciting to see new discoveries that have the potential to significantly improve the lives of people suffering from these conditions. ”